Evaluation of Quality of Life in Breast Cancer Patients: A Cross-Sectional Comparative Study between Targeted Therapy and Conventional Chemotherapy
by Kharisma Jayak Pratama ★ , Niken Luthfiyanti
Academic editor: Mohd Shahezwan Abd Wahab
Sciences of Pharmacy 4(4): 313-321 (2025); https://doi.org/10.58920/sciphar0404453
This article is licensed under the Creative Commons Attribution (CC BY) 4.0 International License.
22 Sep 2025
22 Oct 2025
11 Nov 2025
25 Dec 2025
Abstract: Breast cancer is one of the most common cancers worldwide, with treatment often involving conventional therapies such as chemotherapy. Although effective, chemotherapy is often accompanied by significant side effects and reduces patients' quality of life. Targeted therapy, which targets specific molecular mechanisms in cancer cells, offers the potential to address these issues with higher efficacy and fewer side effects. This study aims to compare the quality of life of breast cancer patients receiving targeted therapy with chemotherapy. The study design used a comparative cross-sectional design involving 60 patients (30 receiving targeted therapy, 30 receiving chemotherapy) selected via consecutive sampling at RSUD Moewardi in Surakarta (January–June 2025). Data were collected using the validated Indonesian version of the EORTC QLQ-C30 questionnaire. Statistical analysis included parametric t-tests and non-parametric Mann-Whitney U tests. The study results showed that the targeted therapy group had better role functioning (p = 0.047.95% CI=0.044-0.053) and significantly lower pain (p= 0.001.95% CI=0.000-0.002) and nausea (p = 0.019.95% CI=0.016-0.021) symptoms compared to chemotherapy. Global health status did not differ significantly (p= 0.545.95% CI=0.536-0.556). Age (p = 0.012.95% CI=0.08-0.012) and stadium (p = 0.001.95% CI=0.001-0.003) significantly influenced global QoL. Targeted therapy provided advantages in functional aspects and specific symptoms, although not in global QoL. A key study limitation is its cross-sectional design, which prevents the establishment of causal relationships between the type of therapy and quality of life outcomes.
Keywords: Breast cancerQuality of lifeTargeted therapy
Introduction
Cancer is the leading cause of death globally and is a non-communicable disease with an increasing trend in cases (1). In 2020, there were 19.2 million new cases of cancer worldwide, with 9.9 million deaths (2). According to the Global Cancer Observatory (2020), breast cancer ranks first in new cancer cases (2.2 million cases) and is the most common cancer in Indonesia (65.000 cases) (3). This cancer predominantly affects women (22% of all female cancers) and is the second leading cause of death after lung cancer (4). The highest incidence rate is found in the 40–49 age group, while those under 35 account for less than 5%. Breast cancer in men is sporadic rare (<1% of total cases) (5). His increase is driven by changes in lifestyle and advancements in diagnostic technology for malignant tumors (6).
Conventional treatments such as chemotherapy, radiation therapy, and surgery have proven effective in controlling the disease, but often cause significant side effects, reduced quality of life, fatigue, nausea, and impaired bodily functions (7). As an alternative, targeted therapy has emerged, which works by inhibiting specific molecules (such as HER2 or hormone receptors) in cancer cells. This therapy is primarily used for the HR+/HER2- (hormone receptor-positive/HER2-negative) subtype (8). According to the National Comprehensive Cancer Network (NCCN) guidelines, drugs such as trastuzumab, pertuzumab, T-DM1, and lapatinib are recommended for neoadjuvant, adjuvant, and metastatic treatment (9). The conceptual framework states that the selective action of targeted therapy on the HER2 receptor reduces non-specific cytotoxicity, thereby minimizing damage to healthy cells. Mechanistically, chemotherapy non-specifically targets rapidly dividing cells (including healthy cells), whereas targeted therapy is designed to selectively disrupt cancer signaling pathways, thereby theoretically reducing systemic toxicity (10).
Breast cancer patients face multidimensional challenges that extend beyond clinical symptoms, encompassing psychological distress (e.g., anxiety, depression), social impacts (e.g., stigma, changes in family roles), and physical sequelae (e.g., sexual dysfunction, body image changes) (11). In this context, quality of life (QoL) is a critical outcome measure, especially given the chronic nature of breast cancer and the need for long-term treatment. QoL is not merely a supportive factor but a key indicator of holistic therapeutic success (12).
While targeted therapy is theorized to offer a better side-effect profile, empirical evidence comparing its impact on QoL directly against conventional chemotherapy remains limited and sometimes inconsistent. For instance, while some studies on newer agents demonstrate promising outcomes, research interpreting QoL scores in specific breast cancer contexts is still developing (13). Conversely, other recent real-world studies provide evidence that targeted therapies, such as CDK4/6 inhibitors, can maintain patients' quality of life over extended periods, highlighting their potential advantage (14). This body of evidence underscores the need for more direct comparative studies. Furthermore, there is a distinct lack of such data from Southeast Asian populations, where cultural, economic, and healthcare system differences may uniquely influence patient-reported outcomes. This gap is critical, given the high cost of targeted therapy and the need to justify its value not just by survival but also by patient-centric outcomes like QoL.
Against this backdrop, this study aims to specifically compare the mean scores of key QoL domains including global health status, role functioning, and symptom scales such as pain and nausea between breast cancer patients receiving targeted therapy and those receiving conventional chemotherapy. We hypothesize that patients receiving targeted therapy will report significantly better outcomes in specific functional and symptom domains compared to those receiving chemotherapy. The results are expected to provide scientific evidence to guide clinicians in selecting treatment regimens that not only extend life expectancy but also maintain patients' optimal quality of life.
Methodology or Experimental Section
Study Design and Research Subjects
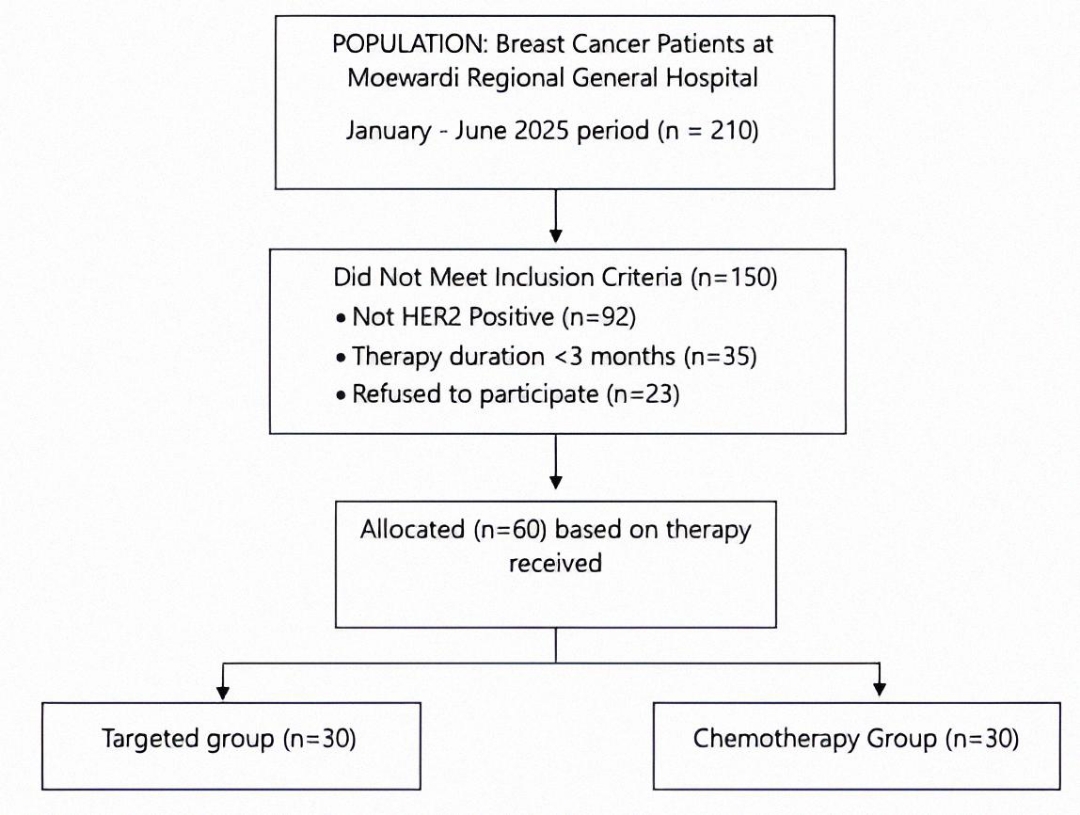
This study used a comparative cross-sectional design to compare the quality of life of breast cancer patients receiving targeted therapy versus conventional chemotherapy. However, it is important to note that as a cross-sectional study, this design can identify associations between therapy type and quality of life outcomes but cannot establish causal relationships due to the lack of temporal sequence assessment and potential unmeasured confounding.The study was conducted at the Oncology Outpatient Clinic of Moewardi General Hospital from January to June 2025. Subjects were selected using consecutive sampling, which included all outpatients who met the inclusion criteria during the study period. Inclusion criteria included: histologically confirmed diagnosis of breast cancer, HER2-positive status (specifically for the targeted therapy group receiving a trastuzumab-based regimen), minimum therapy duration of 3 months, treatment in an adjuvant or first-line metastatic setting, age ≥18 years, and written informed consent. Exclusion criteria were central nervous system metastasis, severe comorbidities, cognitive impairment, multiple malignancies, or pregnancy. Of the 210 patients screened, 150 did not meet the criteria and 60 patients were ultimately recruited (Figure 1). Participants were allocated into two groups: 30 patients received targeted therapy and 30 patients received conventional chemotherapy.
Administrative and Ethical Approval
Ethical approval was obtained from the Moewardi General Hospital Ethics Committee (Reference: 1.277/VI/HREC/2025). Administrative permission was secured to access medical records and administer questionnaires. All participants provided written informed consent after receiving comprehensive study information. Data confidentiality was maintained through anonymization and secure storage.
Data Source
Data collection integrated medical record reviews and structured interviews using the Indonesian version of EORTC QLQ-C30 questionnaire, validated by Perwitasari et al. (2011) (15). Clinical data included disease stage, treatment type, and duration. Quality of life assessment covered global health status, functional scales (physical, role, emotional, cognitive, social), and symptom scales (fatigue, pain, nausea/vomiting). Questionnaire administration followed standardized protocols to minimize interviewer bias. The measurement of quality of life using the EORTC QLQ-C30 questionnaire results consists of two stages. The first stage involves calculating the raw score for each scale using Equation 1. The second stage is the linear transformation stage, which involves standardizing the raw scores to obtain a score range of 1-100 using the linear transformation formula as seen in Equation 2 and 3. Scores for all items range from 1 to 4, so the range is 3, except for items contributing to global health status (QoL), which are 7-point questions, so the range is 6 (16).
Data Analysis
Statistical analysis was performed using SPSS version 27. Data normality was evaluated using the Shapiro-Wilk test. The results showed that the data for the Physical Function domain were normally distributed (p > 0.05). Conversely, data for other quality of life domains (including role function, emotional, cognitive, and social function, fatigue, pain, nausea, and other symptoms) were not normally distributed (p < 0.05). Initial intergroup comparisons for all EORTC QLQ-C30 domains used the independent t-test for normally distributed data and the Mann-Whitney U test for non-normally distributed data. To confirm that the significant findings from the initial tests were valid, an Analysis of Covariance (ANCOVA) was performed to examine the relationship between patient age and stadium with Global Health Status. A significance level of p < 0.05 was applied to all analyses.
Result and Discussion
Most respondents were aged 41–59 years (55%) (Table 1), reflecting the epidemiological pattern of breast cancer in Indonesia, where the median age at diagnosis is 51 years (17). These findings are consistent with the characteristics of breast cancer in developing countries, where 70-80% of new cases are diagnosed before the age of 60 (18). The proportion of elderly patients (>60 years) is also quite significant (27%), indicating that breast cancer remains an important issue in the geriatric population, with specific needs in terms of therapeutic approaches (19). From an educational perspective, the majority of patients had a secondary education (junior high school–high school, 71%), indicating low health literacy that could affect their understanding of the disease and treatment decisions. A systematic review from the Middle East noted that higher education levels are consistently associated with better quality of life in breast cancer patients. A possible explanation is that highly educated women tend to better understand their condition and adhere to treatment recommendations, while those with lower education levels are more likely to delay diagnosis and present at an advanced stage at the time of diagnosis (20). Studies in Taiwan also show that educational level and disease stage are significant predictors of physical and mental quality of life in breast cancer survivors. Type of education and stage affect literacy and hence quality of life (21).
Most patients were housewives (48%), followed by entrepreneurs and informal workers. This is important because social and economic support greatly affects psychosocial resilience and financial burden during cancer therapy (22). In terms of clinical stage, most patients were in stage III (52%), reflecting delays in early detection and treatment. Studies in Southeast Asia show that more than 40% of breast cancer patients first visit health services when they are already in an advanced stage (23), which will impact treatment choices, prognosis, and quality of life for patients. Tumor size is also quite large; 53% of respondents had tumors measuring 6–10 cm, and 28% had tumors larger than 10 cm. Large tumor size is often associated with poor prognosis, higher pain levels, and physical functional limitations (24). Histopathologically, invasive ductal carcinoma (IDC) is the most common type of breast cancer, accounting for approximately 55–80% of all invasive breast cancer cases according to WHO classification and current epidemiological data (25). The finding that the majority of patients in the study sample had IDC (57%) is consistent with this global pattern.
Based on the results of a study using the EORTC QLQ-C30 instrument, it was found that breast cancer patients undergoing targeted therapy generally have a better quality of life than those undergoing chemotherapy. This is reflected in higher function scores and lower symptom scores in the targeted therapy group (Table 2). The results show that most function and symptom domains show differences between the two therapy groups, although not all of them are statistically significant.
Physical, social, cognitive, and emotional functions did not show statistically significant differences, but the targeted therapy group consistently performed better than the chemotherapy group. This can be explained by the nature of targeted therapy, which works more selectively on cancer cells, resulting in fewer side effects compared to conventional chemotherapy, which is cytotoxic to all rapidly dividing cells, including healthy cells. Research by Adamowicz (2020) states that there is no significant relationship between performance scales in breast cancer patients before and after chemotherapy (26). Therapies such as trastuzumab and lapatinib, which are commonly used as targeted therapies in HER2-positive patients, have a milder toxicity profile and good tolerability, enabling patients to maintain their daily functions more stably. This is supported by Adamowicz et al. (2020), who found that the highest role and physical function scores were observed in patients receiving hormonal or targeted therapy, while the lowest scores were seen in the chemotherapy group. According to Gluz et al. (2025), targeted therapy does tend to preserve these functions better than conventional chemotherapy, but significant differences often only become apparent over longer periods or in specific subpopulations (e.g., HER2+) (27).
Role functioning showed statistically significant differences, with higher scores in the targeted therapy group (68.89 ± 7.86) compared to chemotherapy (59.44 ± 14.93) with p-value 0,047 (95% CI=0,044-0,053). This indicates that patients undergoing targeted therapy are better able to perform daily activities and fulfill their social roles. These findings align with the report by Hu et al (2025) in the DESTINY-Breast06 study, which found that targeted therapy such as trastuzumab deruxtecan (T-DXd) delays the decline in role function compared to chemotherapy (28).
The symptom scale includes fatigue, sleep disturbances, appetite, constipation, diarrhea, and respiratory problems. There were no statistically significant differences in these symptoms, although clinically the target therapy group appeared to experience slightly milder symptoms. This may be due to individual variation or the short-term effects of therapy. The reduction in these symptoms contributes greatly to patients' comfort in their daily lives. Conversely, patients undergoing chemotherapy tend to experience moreintense physical symptoms, such as sleep disturbances and decreased appetite. Other studies have shown that symptoms reported by breast cancer patients include fatigue in 10 people (38.9%) and nausea in 21 people (80.8%). Symptoms not present in some patients include pain in 13 patients (50%), decreased appetite and constipation in none of the patients (88.5%), diarrhea in 22 patients (84.6%), sleep difficulties in 21 patients (80.8%), and shortness of breath in 18 patients (69.2%) (29).
Characteristics | Respondents: n (%) | Mean | SD | Median | Therapy | |
Targeted | Chemotherapy | |||||
Age | ||||||
<40 | 11 (18%) | 2.08 | 0.67 | 2.00 | 4 (13%) | 7 (23%) |
41-59 | 33 (55%) | 15 (50%) | 18 (60%) | |||
>60 | 16 (27%) | 11 (37%) | 5 (17%) | |||
Education | ||||||
Elementary School | 12 (20%) | 2.35 | 0.67 | 2.00 | 5 (17%) | 7 (23%) |
Junior high school | 20 (33) | 11 (37%) | 9 (30%) | |||
Senior high school | 23 (38%) | 12 (40%) | 11 (37%) | |||
Bachelor's degree | 5 (8%) | 2 (7%) | 3 (10%) | |||
Occupation | ||||||
Housewife | 29 (48%) | 1.63 | 1.00 | 1.00 | 13 (43%) | 16 (53%) |
Civil servant | 7 (12%) | 3 (10%) | 4 (13%) | |||
Entrepreneur | 19 (32%) | 11 (37%) | 8 (27%) | |||
Laborer | 5 (8%) | 3 (10%) | 2 (7%) | |||
Stadium | ||||||
2 | 14 (23%) | 2.01 | 0.70 | 2.00 | 8 (27%) | 6 (20%) |
3 | 31 (52%) | 15 (50%) | 16 (53%) | |||
4 | 15 (25%) | 7 (23%) | 8 (27%) | |||
Tumor Size | ||||||
<2 cm | 2 (3%) | 3.05 | 0.76 | 3.00 | (0%) | 2 (7%) |
2-5 cm | 10 (17%) | 6 (20%) | 4 (13%) | |||
6-10 cm | 31 (53%) | 20 (67%) | 11 (37%) | |||
>10 | 17 (28%) | 4 (13%) | 13 (43%) | |||
Histopathology | ||||||
Ductal | 34 (57%) | 1.43 | 0.49 | 1.00 | 16 (53%) | 18 (60%) |
Non-Ductal | 26 (43%) | 14 (47%) | 12 (40%) | |||
Note: Age coded as 1 = <40, 2 = 41-59, 3 = >60; Education coded as 1 = Elementary, 2 = Junior High, 3 = Senior High, 4 = Bachelor; Occupation coded as 1 = Housewife, 2 = Civil Servant, 3 = Entrepreneur, 4 = Laborer; Stadium coded as 2 = Stage II, 3 = Stage III, 4 = Stage IV; Tumor Size coded as 1 = <2 cm, 2 = 2-5 cm, 3 = 6-10 cm, 4 = >10cm; Histopathology coded as 1 = Ductal, 2 = Non-Ductal. | ||||||
Pain and nausea scores were significantly lower in the targeted therapy group than in the chemotherapy group, indicating that patients receiving targeted therapy experienced fewer complaints of pain and nausea. This is consistent with the findings of Adamowicz et al. (2020), who stated that trastuzumab therapy had a better effect in reducing physical symptoms such as pain and nausea than chemotherapy (26). Similarly, these findings are consistent with a study by Rugo et al. (2022), which also confirmed that targeted agents such as trastuzumab deruxtecan significantly reduce grade ≥3 nausea (30).
Financial distress scores remained high in both groups (mean >40 on a scale of 0–100), indicating that financial toxicity is a systemic burden that transcends the type of therapy. These high scores reflect the cumulative impact of direct (treatment) and indirect (loss of income) costs, which significantly erode patients' well-being. Carrera's analysis (2018) demonstrated that 73% of cancer patients experience severe financial distress, with the greatest impact on treatment adherence (β = -0.78; p = 0.002) and mental health (β = -0.82; p < 0.001) (31). Better symptom control and improved functional outcomes from targeted therapy must be balanced against its economic implications, particularly in resource-limited healthcare systems such as Indonesia. Although not directly measured in this study, high financial hardship scores in both groups (mean >40) highlight the significant economic burden of breast cancer treatment. Targeted therapies, such as trastuzumab, are considerably more expensive than conventional chemotherapy regimens. These costs pose a major challenge to accessibility and equity, as they may only be covered forsome patients with specific insurance or through hospital budget allocations, potentially exacerbating inequalities in healthcare. Although our findings indicate a better side effect profile for targeted therapy, formal cost-benefit analysis is essential to determine its value for money in the Indonesian context. Policymakers and healthcare providers must weigh the improvement in quality of life in specific areas against the high cost of drug acquisition to make informed decisions about funding and priorities within the national health insurance scheme (JKN).
Scale | Target | Chemotherapy | P-Value (95% CI) | ||
Average ± SD | Median | Average ± SD | Median | ||
Functionala | |||||
Physical Function | 75.11 ± 11.21 | 73.00 | 73.33 ± 15.34 | 73.00 | |
Role Function | 68.86 ± 17.26 | 67.00 | 59.56 ± 12.24 | 67.00 | 0.047 (0.044-0.053) |
Emotional Function | 71.43 ± 13.61 | 75.00 | 68.90 ± 8.45 | 67.00 | 0.331 (0.327-0.346) |
Cognitive Function | 79.44 ± 14.83 | 83.00 | 77.20 ± 14.69 | 83.00 | 0.590 (0.606-0.625) |
Social Function | 74.50 ± 15.49 | 67.00 | 78.23 ± 10.65 | 83.00 | 0.207 (0.205-0.221) |
Symptom Scalesb | |||||
Fatigue | 51.66 ± 9.74 | 56.00 | 55.20 ± 13.18 | 56.00 | 0.339 (0.331-0.349) |
Pain | 11.86 ± 9.01 | 17.00 | 23.30 ± 14.78 | 25.00 | 0.001 (0.000-0.002) |
Nausea | 34.26 ± 11.49 | 33.00 | 45.53 ± 20.56 | 50.00 | 0.019 (0.016-0.021) |
Sleep Disturbances | 26.50 ± 20.34 | 33.00 | 25.43 ± 22.65 | 33.00 | 0.784 (0.808-0.823) |
Loss of Appetite | 41.13 ± 25.98 | 33.00 | 38.86 ± 25.06 | 33.00 | 0.703 (0.730-0.748) |
Constipation | 19.86 ± 20.66 | 33.00 | 29.86 ± 22.12 | 33.00 | 0.076 (0.084-0.095) |
Diarrhea | 23.10 ± 15.38 | 33.00 | 22.06 ± 20.16 | 33.00 | 0.676 (0.695-0.713) |
Respiratory Problems | 12.10 ± 16.17 | 0.00 | 20.03 ± 28.61 | 0.00 | 0.505 (0.495-0.515) |
Financial Problems | 43.26 ± 20.11 | 33.00 | 47.76 ± 19.23 | 33.00 | 0.87 (0.441-0.461) |
Global Health Status/Quality of Lifea | 74.43 ± 19.39 | 75.00 | 71.70 ± 16.96 | 67.00 | 0.545 (0.536-0.556) |
The global quality of life score for targeted therapy was higher (74.44 ± 19.44) than for chemotherapy (71.67 ± 17.04), but this difference was not statistically significant p = 0.545, (95% CI=0,536-0,556). While the observed differences in role functioning, pain, and nausea were statistically significant, their clinical meaning—the extent to which a patient would perceive a meaningful change in their daily life—requires further interpretation. According to established guidelines for the EORTC QLQ-C30, a difference of 5-10 points is often considered a small change, while a difference of 10-20 points represents a moderate to large change that is likely to be clinically relevant from the patient's perspective (32). The differences we observed in role functioning (approximately 9 points), pain (approximately 11 points), and nausea (approximately 11 points) suggest a potential clinical benefit for targeted therapy, particularly for pain and nausea where the difference exceeds the 10-point threshold. In contrast, the non-significant difference of less than 3 points in Global Health Status further supports the conclusion that patients' overall perception of their health was not meaningfully different between the two groups. This distinction underscores the importance of evaluating both statistical p-values and the magnitude of score differences to fully appreciate the real-world impact of a therapy on patient well-being. A study by Gayatri (2020) on 1,203 patients with metastatic breast cancer demonstrated that significant changes in Global Health Status generally require consistent improvements across multiple domains (physical, emotional, social) over a period of >6 months (33). Another study noted that the Health-Related Quality of Life (HRQOL) of patients treated with chemotherapy alone was significantly lower compared to patients treated with hormonal therapy or targeted therapy (0.76 vs. 0.82 or 0.85; p = 0.0020) (34).
Characteristics | Test Statistic | (95% CI) | p-value |
Age | H= 8.775 | (0.008-0.012) | 0.012 |
Education | H= 2.674 | (0.439-0.459) | 0.445 |
Occupation | H = 5.261 | (0.141-0.155) | 0.154 |
Stadium | H= 13.803 | (0.001-0.003) | 0.001 |
Tumor Size | H = 5.484 | (0.130-0.144) | 0.140 |
Histopathology | U= 429.000 | (0.842-0.856) | 0.841 |
Note: The significant differences are in bold. H= Kruskal-Wallis Test, U= Mann-Whitney U Test, CI confidence interval. | |||
Characteristics | Adjusted Mean ± SE | F-value | p-value | Partial η² | 95% CI |
Education | |||||
Elementary | 76.28 ± 4.95 | 1.039 | 0.383 | 0.055 | 66.36-86.20 |
Junior High | 72.35 ± 3.73 | 64.88-79.83 | |||
Senior High | 69.72 ± 3.50 | 62.69-76.74 | |||
Bachelor | 83.62 ± 8.29 | 67.01-100.24 | |||
Occupation | |||||
Housewife | 73.76 ± 2.76 | 0.071 | 0.975 | 0.004 | 68.22-79.30 |
Civil servant | 71.06 ± 8.13 | 54.76-87.36 | |||
Entrepreneur | 72.56 ± 6.09 | 60.36-84.77 | |||
Laborer | 71.13 ± 8.37 | 54.35-87.91 | |||
Histopathology | |||||
Ductal | 69.47 ± 2.89 | 3.279 | 0.076 | 0.055 | 63.68-75.26 |
Non-Ductal | 77.77 ± 3.34 | 71.08-84.47 | |||
Tumor Size | |||||
< 2 cm | 72.89 ± 12.79 | 0.596 | 0.620 | 0.032 | 47.24-98.54 |
2 – 5 cm | 80.29 ± 5.99 | 68.28-92.31 | |||
6 – 10 cm | 71.63 ± 3.10 | 65.42-77.85 | |||
>10 cm | 71.44 ± 5.08 | 61.25-81-62 | |||
Age | |||||
<40 | 69.51 ± 6.88 | 0.163 | 0.850 | 0.006 | 55.72-83.30 |
41-59 | 73.68 ± 2.91 | 67.84-79.53 | |||
>50 | 74.22 ± 5.59 | 63.02-85.42 | |||
Stadium | |||||
2 | 59.69 ± 6.04 | 2.868 | 0.65 | 0.093 | 47.57-71.80 |
3 | 75.81 ± 2.95 | 69.89-81.73 | |||
4 | 79.86 ± 5.65 | 68.53-91.19 | |||
Note: SE = Standard Error, Partial η² = Effect Size (0.01 = small, 0.06 = medium, 0.14 = large), CI confidence interval. Analysis of Covariance (ANCOVA) controlling for age and disease stage. | |||||
Table 3 shows that there is a significant relationship between patient age and overall quality of life. A p-value 0,012 (95% CI=0,08-0,012) of less than 0.05 indicates that age affects patient quality of life. This finding is influenced by physiological factors such as reduced organ reserve capacity and frailty syndrome in older patients, which reduce their tolerance to treatment side effects, psychosocial factors such as better adaptation to social role and work changes in younger patients, and the burden of comorbidities, with a prevalence of comorbidities three times higher in the >65 age group. The study by Rini et al. (2022) on 2,189 breast cancer patients demonstrated that patients under 50 years of age had a 18-point higher physical function score (95% CI 12.4–23.6) and a 40% lower risk of emotional distress (OR 0.6; p=0.01) compared to the group over 65 years of age (35).
Educational characteristics are not significantly related to overall quality of life. Although education can influence patients' understanding of their disease and treatment, in this case there appears to be no direct effect on their quality of life. Other factors such as social support or anxiety levels may play a greater role in determining patients' quality of life. Other studies suggest that patient education has a significant effect on short-term overall quality of life, emotional quality of life, and fatigue, although all results are classified as 'not important' (36).
The study showed no significant relationship with overall quality of life (p=0.154), but there were indications that patients who were employed had a slightly better quality of life than those who were not. However, a p-value greater than 0.05 indicates that this difference is not statistically significant. Other research has found that a cancer diagnosis puts a person at risk for poor work outcomes, including job loss with accompanying financial toxicity and related consequences, such as bankruptcy, poor symptom control, reduced quality of life, treatment noncompliance, and premature death (37).
The stadium of the disease was found to have a highly significant association with patients' quality of life p-value = 0.001, (95% CI=0,001-0,003). Patients with more advanced stages (stadium III and IV) demonstrated lower quality of life compared to patients with earlier stages. The decline in quality of life in advanced stages is attributed to: heavier symptom burden such as pain, fatigue, and metastatic complications; higher treatment intensity such as cumulative side effects of aggressive therapy; and psychosocial burden including anxiety about prognosis and functional disability. Another study noted that regression analysis revealed that clinical factors associated with lower quality of life include disease progression, chemotherapy, and side effects such as hair loss or stomatitis (34).
Tumor size did not show a significant relationship with global quality of life (p = 0.140). This lack of significance can be explained by the dominance of non-tumor factors, including type of therapy, individual biological response, and psychosocial support. The dissociation between objective and subjective parameters—specifically, tumor size does not linearly correlate with symptom burden—and the mediating effect of treatment. An effective therapy regimen can compensate for the impact of a large tumor. Other studies indicate that tumor size is not the only factor influencing patient fitness and survival (38). Although tumor size is important in prognosis, other factors such as type of treatment and social support play a greater role in patients' quality of life.
Histopathology also showed no significant association with patients' quality of life (p = 0.841). Although histopathology type may influence clinical prognosis, other factors such as the therapy administered and patients' response to treatment appear to have a greater impact on patients' quality of life. Other studies have also stated that although histopathology is important in determining treatment, it is not significantly associated with clinical factors.
Based on the results of ANCOVA analysis controlling for the effects of age and stadium (Table 4), most patient characteristics did not show a significant effect on Global Health Status. Demographic characteristics such as education (F=1.039, p=0.383) and occupation (F=0.071, p=0.975) had small effect sizes (η²<0.06), indicating minimal contribution to quality of life variation. Similarly, age (F=0.163, p=0.850) and tumor size (F=0.596, p=0.620) had no significant effect. However, clinical characteristics such as histopathology (F=3.279, p=0.076) and disease stage (F=2.868, p=0.065) showed a trend approaching significance with a medium effect size (η²≈0.09), where non-ductal and advanced stage patients had higher scores.
These findings indicate that clinical factors are more determinative in influencing patients' quality of life than demographic factors. The non-linear pattern in disease stage, where stage IV patients actually reported higher scores (79.86), may reflect psychological adaptation processes or differences in treatment expectations. These results are consistent with the study by Lorusso et al. (2023) that quality of life assessments are multidimensional and do not always correlate directly with objective clinical parameters (32). Therefore, a holistic approach that considers psychosocial aspects remains necessary, even though demographic factors are not statistically significant.
This study has several limitations that should be considered when interpreting the results. First, the use of a consecutive sample from a single tertiary care center may limit the generalizability of the findings to other healthcare settings or patient populations in Indonesia, such as those in primary care facilities or rural regions with different demographic and clinical characteristics. This sampling method may have introduced selection bias, as patients treated at tertiary hospitals often present with more complex or severe conditions.
Second, the cross-sectional design prevents the establishment of causal relationships between therapy type and quality-of-life outcomes because it captures data at a single point in time. Third, the absence of longitudinal follow-up limits the ability to evaluate the stability of the observed QoL differences throughout the treatment course or to assess the long-term impact of these therapies, including late-onset side effects or adaptive changes in patient-reported outcomes. Finally, the relatively short minimum therapy duration of three months may not fully capture the entire spectrum of treatment-related effects on quality of life.
Conclusion
Targeted therapy showed significant differences in role functioning (p = 0.047, 95% CI = 0.044–0.053), pain (p = 0.001, 95% CI = 0.000–0.002), and nausea (p = 0.019, 95% CI = 0.016–0.021) compared to conventional chemotherapy. However, there was no significant difference in overall health status (p = 0.545, 95% CI = 0.536–0.556). Age (p = 0.012, 95% CI = 0.008–0.012) and disease stage (p = 0.001, 95% CI = 0.001–0.003) were statistically significant factors influencing overall quality of life, whereas education level (p = 0.445), occupation (p = 0.154), tumor size (p = 0.140), and histopathology (p = 0.841) were not significant. These findings confirm that although targeted therapy provides advantages in specific functional and symptomatic domains, therapeutic strategies should prioritize patient characteristics particularly age and disease stage to optimize holistic quality of life. Covariance analysis (ANCOVA) controlling for age and disease stage showed that patient characteristics (education, occupation, histopathology, and tumor size) did not significantly affect Global Health Status/Quality of Life (all p > 0.05). This indicates that these variables are not major determinants of overall quality of life in this sample after adjustment.This analytical adjustment also highlights a key limitation of this study: the observed advantages in specific domains may be influenced by unmeasured factors, and the cross-sectional design does not allow causal inference. Therefore, these results should be interpreted as exploratory and hypothesis-generating rather than confirmatory evidence of targeted therapy efficacy. While targeted therapy shows promising benefits in symptom relief and functional status, future longitudinal or randomized controlled clinical trials are essential to validate these associations and establish causality. Clinical decision-making should continue to integrate patient characteristics, treatment effectiveness, symptom burden, and cost-effectiveness.
Declarations
Acknowledgment
Our gratitude goes to the Ministry of Higher Education, Science, and Technology of the Republic of Indonesia (Kemdiktisaintek RI) through the 2025 Beginer Lecturer Research Grant Program and the Research and Institute for Research and Community sevice, Universitas Duta Bangsa Surakarta, so that this activity can be carried out. We would also like to thank Moewardi Regional General Hospital for agreeing to be the location for this research.
Ethics Statement
The Health Research Ethics Committee Dr. Moewardi No: 1.277/VI/HREC/2025
Data Availability
All data generated or analyzed during this study are included in this published article.
Funding Information
This research was funded by the Ministry of Education, Culture, Research, and Technology of the Republic of Indonesia under Grant No: 127/C3/DT.05.00/PL/2025
Conflict of Interest
The authors declare no conflicting interest.
References
- Ayenigbara IO. Risk-Reducing Measures for Cancer Prevention. Korean J Fam Med. 2023;44(2):76.
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020. CA Cancer J Clin. 2021;71(3):209–249.
- Global Cancer Observatory. Breast Cancer Fact Sheet 2020. Lyon: IARC; 2021.
- Arnold M, Morgan E, Rumgay H, et al. Current and future burden of breast cancer. Breast. 2022;66:15–23.
- Cardoso F, Kyriakides S, Ohno S, et al. Early breast cancer: ESMO guidelines. Ann Oncol. 2019;30(8):1194–1220.
- Momenimovahed Z, Salehiniya H. Epidemiological characteristics and risk factors for breast cancer. Breast Cancer. 2019;11:151–164.
- Kaur R, Bhardwaj A, Gupta S. Cancer treatment therapies. Mol Biol Rep. 2023;50:9663–9676.
- Dalal AA, Gagnon-Sanschagrin P, Burne R, et al. Dosing patterns and burden of palbociclib wastage. Adv Ther. 2018;35(6):768–778.
- Kreutzfeldt J, Rozeboom B, Dey N, De P. Targeted HER2+ breast cancer therapies. Am J Cancer Res. 2020;10(4):1045–1067.
- Slamon DJ, Neven P, Chia S, et al. Ribociclib plus fulvestrant. N Engl J Med. 2020;382(6):514–524.
- Dinapoli L, Colloca G, Di Capua B, et al. Psychological aspects in breast cancer. Curr Oncol Rep. 2021;23:38.
- Bottomley A, Flechtner H, Efficace F, et al. QoL outcomes in cancer trials. Eur J Cancer. 2005;41(12):1697–1709.
- Kawahara T, Taira N, Shiroiwa T, et al. Minimal important differences of EORTC QLQ-C30. Qual Life Res. 2022;31(6):1829–1836.
- Rocque GB, Blum JL, Ji Y, et al. QoL with palbociclib: POLARIS. Breast Cancer Res Treat. 2025;209(3):613–627.
- Perwitasari DA, Atthobari J, Dwiprahasto I, et al. Translation and validation of EORTC QLQ-C30 Indonesian. Jpn J Clin Oncol. 2011;41(4):519–529.
- Ratna R, Supadmi W, Yuniarti E. Kualitas hidup pasien kanker. Majalah Farmaseutik. 2021;17(2):278–286.
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020. CA Cancer J Clin. 2021;71(3):209–249.
- Martei YM, Pace LE, Brock JE, et al. Breast cancer in LMICs. Clin Lab Med. 2018;38(1):161–173.
- Fusco D, Ferrini A, Pasqualetti G, et al. Geriatric assessment in cancer. Eur J Clin Invest. 2021;51(1):e13347.
- El Haidari R, Abbas LA, Nerich V, Anota A. QoL in Middle East breast cancer. Cancers. 2020;12(3):696.
- Wei CW, Wu ML, Tung HH. Health literacy and QoL. Int J Nurs Pract. 2021;27(2):e12922.
- Olvera RG, Myers SP, Gaughan AA, et al. Social support and financial toxicity. Cancers. 2025;17(10):1712.
- Lim YX, Lim ZL, Ho PJ, Li J. Breast cancer in Asia. Cancers. 2022;14(17):4218.
- Waks AG, Winer EP. Breast cancer treatment review. JAMA. 2019;321(3):288–300.
- Makki J. Diversity of breast carcinoma. Clin Med Insights Pathol. 2015;8:23–31.
- Adamowicz K, Baczkowska-Waliszewska Z. QoL during chemo, hormonotherapy, anti-HER2. Health Qual Life Outcomes. 2020;18:134.
- Gluz O, Xu B, Nanda R, et al. Sacituzumab versus physician’s choice. Ther Adv Med Oncol. 2025;17:17588359251320285.
- Hu X, Curigliano G, Yonemori K, et al. Patient-reported outcomes trastuzumab deruxtecan. ESMO Open. 2025;10(5):105082.
- Angraini D, Semiarty R, Rasyid R, Khambri D. Faktor yang mempengaruhi kualitas hidup. J Endurance. 2018;3(3):562–567.
- Modi S, Jacot W, Yamashita T, Sohn J, Vidal M, Tokunaga E, et al. Trastuzumab deruxtecan in previously treated HER2-low advanced breast cancer. N Engl J Med. 2022;387(1):9-20.
- Carrera PM, Kantarjian HM, Blinder VS. The financial burden and distress of patients with cancer: understanding and stepping-up action on the financial toxicity of cancer treatment. CA Cancer J Clin. 2018;68(2):153-165.
- Lorusso D, Colombo N, Casado Herraez A, Santin AD, Colomba E, Miller DS, et al. Health-related quality of life in patients with advanced endometrial cancer treated with lenvatinib plus pembrolizumab or treatment of physician’s choice. Eur J Cancer. 2023;186:172-184.
- Gayatri D, Efremov L, Kantelhardt EJ, Mikolajczyk R. Quality of life of cancer patients at palliative care units in developing countries: systematic review of the published literature. Qual Life Res. 2021;30(2):315-343.
- Park M, Yu SY, Jeon HL, Song I. Factors affecting health-related quality of life in patients with metastatic breast cancer. J Breast Cancer. 2023;26(5):436-445.
- Rini C, Waltz M, Bovbjerg K, Farrell D, Yanez B, Chicaiza A, et al. Optimizing use of written peer support as a supportive resource in cancer: focus group insights. Psychooncology. 2022;31(9):1589-1596
- Martínez-Miranda P, Casuso-Holgado MJ, Jiménez-Rejano JJ. Effect of patient education on quality-of-life, pain and fatigue in breast cancer survivors: a systematic review and meta-analysis. Clin Rehabil. 2021;35(12):1722-1742.
- Blinder VS, Gany FM. Impact of cancer on employment. J Clin Oncol. 2020;38(4):302-309.
- Ayuza M, Harahap WA, Rustam R, Nindrea RD. Faktor yang berpengaruh terhadap disease free survival dan overall survival pada pasien kanker payudara usia muda di Kota Padang tahun 2008–2018. J Kesehat Andalas. 2020;9(1S).

 ETFLIN
Notification
ETFLIN
Notification






