Nanochemistry in Vaccine Delivery: Lipid Nanoparticles, Polymers, and Hybrid Systems
by Courage Chandipwisa ★ , Agness Shimilimo , Tendai Pride Zenda , Harrison Banda
Academic editor: Adeleye Ademola Olutayo
Sciences of Pharmacy 5(1): 22-33 (2026); https://doi.org/10.58920/sciphar0501525
This article is licensed under the Creative Commons Attribution (CC BY) 4.0 International License.
07 Dec 2025
07 Jan 2026
12 Jan 2026
19 Jan 2026
Abstract: Conventional vaccines face challenges in antigen stability, delivery efficiency, and scalability, particularly in low- and middle-income countries. Nanochemistry offers innovative approaches through lipid nanoparticles, polymeric carriers, and hybrid systems. This review evaluates these platforms using criteria such as physicochemical properties, immunological outcomes, translational feasibility, and One Health relevance. A narrative literature review was conducted across major databases between 2015 and 2025. Studies were screened by title and abstract, excluded if not directly relevant to vaccine delivery, and weighted according to design, with clinical trials prioritized over in vitro or modeling studies. Reference lists of key papers were also examined to ensure comprehensive coverage. Lipid nanoparticles supported mRNA delivery in licensed COVID-19 vaccines, achieving strong immune responses but with variability across populations and reported adverse events including myocarditis and anaphylaxis. Polymeric nanoparticles such as PLGA and chitosan enabled controlled antigen release, though cost-effectiveness remains constrained by manufacturing and scalability challenges. Hybrid lipid-polymer systems demonstrated enhanced stability and multi-antigen presentation, with current evidence largely limited to preclinical studies. One Health implications are defined as the potential of nanochemistry to contribute to zoonotic disease prevention, food safety, and cross-species vaccine design, requiring clearer frameworks for integration. In conclusion, nanochemistry-based vaccine platforms show promise for advancing immunization strategies, but unresolved issues in safety evaluation, regulatory harmonization, and equitable access highlight the need for cautious interpretation and further interdisciplinary collaboration.
Keywords: NanochemistryVaccine deliveryLipid nanoparticles
Introduction
Vaccination remains one of the most effective public health interventions, yet conventional platforms continue to face problems of antigen instability, inefficient delivery, and limited scalability, particularly in low- and middle-income countries (LMICs) (1). These challenges underscore a clear knowledge gap: while nanochemistry has advanced rapidly, there is no comprehensive synthesis that critically evaluates lipid, polymeric, and hybrid nanoparticle systems in vaccinology (2). Adverse reactions and vaccine failure have been reported, this review situates such outcomes within specific contexts. For example, the incidence of anaphylaxis following mRNA vaccination has been estimated at 4.7 cases per million doses for Pfizer-BioNTech and 2.5 per million for Moderna (3). Myocarditis has been observed at 12.6 cases per million second doses among individuals aged 12-39 years (4). These data highlight the importance of contextualizing safety outcomes. mRNA vaccines are correctly described as being produced through in vitro transcription, not “ex vivo transcription.” Despite their promise, mRNA molecules remain vulnerable to RNase degradation and face barriers to cellular uptake due to size and polarity (5). Nanotechnology and nanomedicine have been widely applied in diagnostics and therapeutics, they are explicitly linked to vaccinology challenges: stabilizing fragile antigens, enhancing immune modulation, and enabling precise delivery to antigen-presenting cells (6). The COVID-19 pandemic accelerated vaccine science, not only by validating mRNA-lipid nanoparticle platforms at scale but also by reshaping regulatory pathways, manufacturing capacity, and global equity debates (7-8). The aim of this paper is therefore to provide a critical synthesis of nanochemistry-based vaccine platforms, evaluating their physicochemical properties, immunological outcomes, translational feasibility, regulatory challenges, and One Health implications.
Methodology
This review was conducted as a structured narrative synthesis of published and grey literature on nanochemistry-based vaccine platforms. To ensure transparency, explicitprocedures for study identification, screening, exclusion, and risk-of-bias assessment were defined prior to data extraction. Electronic searches were performed in PubMed, Scopus, Web of Science, and Google Scholar between 2015 and 2025. Search strings combined controlled vocabulary and free-text terms, including “nanochemistry AND vaccine,” “lipid nanoparticle AND mRNA,” “polymeric nanoparticle AND immunization,” and “hybrid nanoparticle AND vaccine delivery.” Reference lists of key articles were hand-searched to identify additional studies. Titles and abstracts were screened independently by two reviewers. Full texts were retrieved for potentially eligible studies, and disagreements were resolved by consensus. Exclusion criteria included studies lacking primary data, those focused solely on diagnostic nanotechnology, and opinion pieces without methodological detail. Grey literature was included to capture regulatory reports, WHO technical briefs, and industry white papers relevant to translational feasibility. Quality control measures involved assessing source credibility, publication venue, and methodological transparency before inclusion. Thematic synthesis was applied prospectively to guide the structure of the review. Themes were defined a priori as: (i) lipid nanoparticles, (ii) polymeric nanoparticles, (iii) hybrid systems, (iv) translational and regulatory challenges, and (v) One Health implications. The risk-of-bias was assessed using adapted Cochrane criteria for clinical studies and ARRIVE guidelines for animal studies. Heterogeneity was evaluated by comparing outcomes across study designs (in vitro, animal models, clinical trials). Conflicting findings were highlighted, and strength of evidence was graded using a modified GRADE approach, prioritizing randomized controlled trials and large cohort studies over preclinical data. Table 1 summarizes the criteria. Inclusion required explicit focus on vaccine delivery using nanochemistry-based systems, reporting of immunological outcomes, and sufficient methodological detail. Exclusion applied to studies lacking primary data or those not addressing vaccine delivery.
S/N | Criteria | Inclusion | Exclusion |
1 | Publication type | Peer-reviewed journal articles, reviews, clinical trial reports, and experimental studies. | Non-peer-reviewed articles, opinion pieces, blogs, and news reports. |
2 | Time frame | 2015-2025. | Studies published before 2015. |
3 | Language | English. | Non-English publications without translation. |
4 | Content focus | Studies on nanochemistry-based vaccine delivery (lipid nanoparticles, polymers, hybrid systems). | Studies focusing solely on non-vaccine drug delivery systems. |
5 | Study design | In vitro, in vivo, clinical trials, modeling, and translational studies. | Studies without relevance to immunology or vaccine delivery. |
6 | Population | Human and animal studies relevant to vaccine applications. | Studies restricted to material science without immunological context. |
7 | Risk of bias | Studies assessed with Cochrane/ARRIVE criteria, low to moderate bias acceptable. | High risk of bias, unclear methodology. |
8 | Evidence grading | RCTs, large cohort studies prioritized; GRADE applied. | Opinion pieces, narrative reviews without primary data. |
9 | Nanoparticle characterization | Explicit reporting of particle size, charge, composition. | Studies lacking physicochemical detail. |
Results
Principles of nanochemistry in vaccinology
Nanochemistry is an emerging sub-discipline of the chemical and material sciences that deals with the development of new methods for creating nanoscale materials. The physiochemical properties of particles are key to the utility of nano-adjuvants in preclinical research. The change of particle size, shape, surface charge, ligand density, and rigidity can cause changes in immune efficiency. Size, shape, and surface chemistry have effects on the immunological response and the administration routes and diversification of adjuvant potency.
Size effect
Nanomaterials (chemical substances or materials with one dimension at least 1 to 100 nm in size) have been studied for their roles in regenerative medicine and vaccine delivery. The size of particles can influence interactions at the cell-biological interface, but outcomes vary depending on antigen type, delivery route, and host species. Particles may enter antigen-presenting cells (APCs) through pinocytosis, phagocytosis, or other uptake mechanisms. For example, particles internalized by M cells are generally below 1 μm, whereas uptake by small intestine epithelial cells is often reported for particles <500 nm (9). Particles <150 nm are frequently observed to enter cells through pinocytosis, while larger vesicles (>250 nm) are more often associated with phagocytosis (10). The size of particles also indirectly alters surface curvature and specific surface area, which can affect uptake efficiency. Internalization by APCs is important for antigen expression, but does not guarantee high immunogenicity. Some studies suggest that particles >500 nm are more likely to enter early lysosomes and associate with MHC II, which has been linked to Th2‑biased responses, while smaller particles (<200 nm) may escape into the cytoplasm and be loaded into MHC I, supporting CD8+ T cell activation and Th1‑biased responses (11). However, contradictory findings exist, with several reports showing mixed or absent polarization effects, indicating that particle size alone does not determine immune outcome (12, 13). Activation of signaling pathways and cytokine secretion also differ according to particle size and biological context, with variability across experimental systems (14).
Charge and surface chemistry
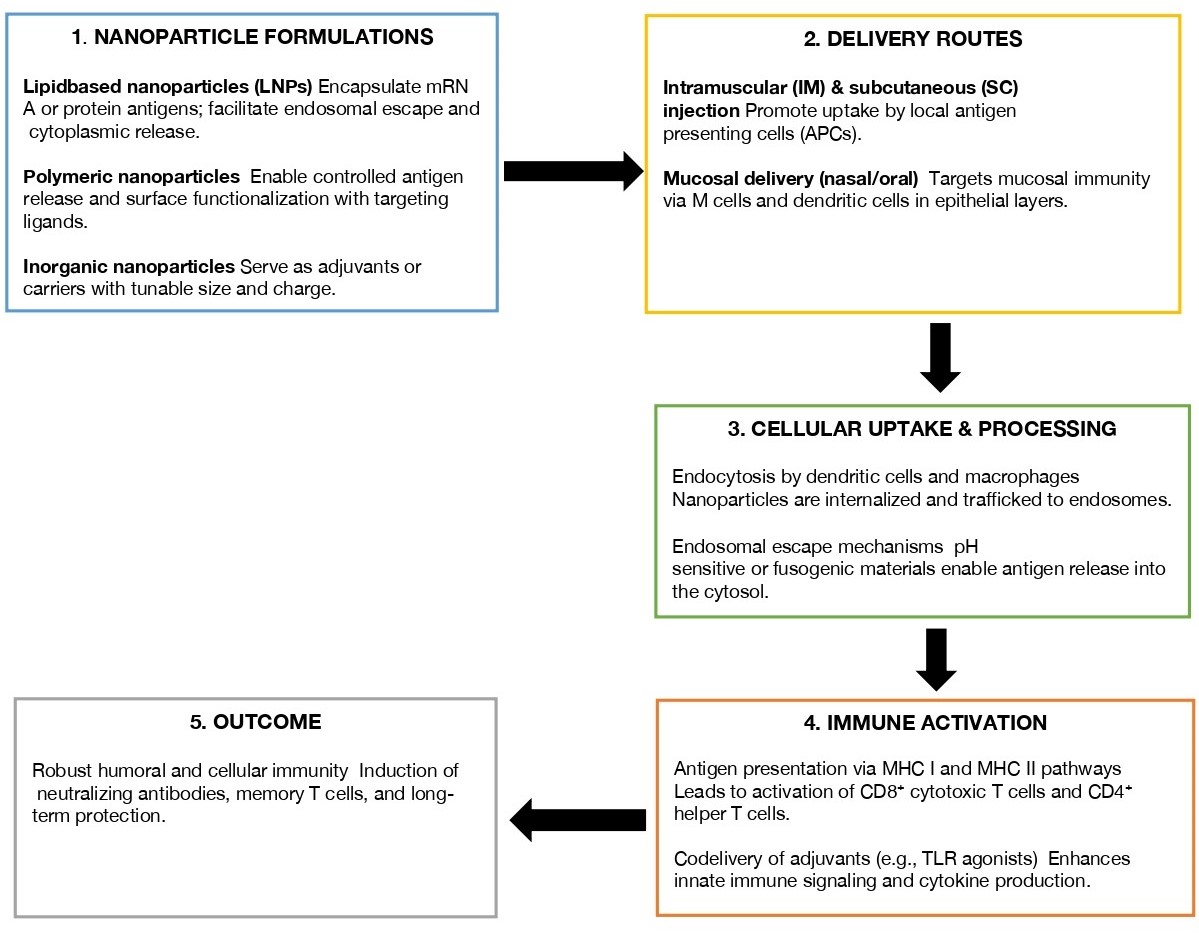
The surface chemistry of nanoparticles (NPs) influences their behavior in physiological media, but immune outcomes are not deterministic. Surface charge affects circulation, uptake, and immune signaling. Positively charged gold NPs have been reported to activate ERK and JNK pathways, producing pro‑inflammatory and anti‑inflammatory factors, while negatively charged particles are often internalized through receptor‑dependent pathways and associated with TNF‑α release via ERK signaling (15). Positively charged NPs are frequently linked to higher ROS generation and lysosomal disruption, which can support Th1 responses and CD8+ T cell activation (16). However, other studies have reported minimal or opposite effects, with negatively charged particles also capable of inducing pro‑inflammatory cytokines depending on formulation (17, 18). Surface modification of NPs can influence macrophage polarization and T helper cell differentiation, but findings are inconsistent across different systems, highlighting the need to interpret these pathways as context‑dependent rather than deterministic. For example, Sun et al. reported that NH2‑functionalized aluminium oxyhydroxide nanorods showed higher uptake and oxidative stress compared with SO3H‑functionalized nanorods (19), yet other studies have observed variable outcomes depending on ligand density and spacing (20). Particle shape anisotropy also plays a role, with rod‑shaped NPs sometimes showing preferential uptake and TNF‑α secretion (21), but contradictory evidence suggests that immune stimulation is influenced by multiple interacting factors rather than determined by a single property. Figure 1 provides a schematic representation of how nanoparticle formulations may be delivered, absorbed, and processed before activating host immune mechanisms.
Lipid nanoparticles
Lipid nanoparticles (LNPs) have emerged as a game-changer RNA delivery system. This is because LNPs can transport intact mRNA from the application site into the cytoplasm, where translation can occur (22). LNPs are typically composed of four essential components: an ionizable lipid, a phospholipid, cholesterol, and PEG-lipid conjugates. Each of these lipids plays a crucial role in efficient intracellular delivery. DNA vaccine is an attractive immune platform for the prevention and treatment of infectious diseases, but existing disadvantages limit its use in preclinical and clinical assays, such as weak immunogenicity and short half-life. In one preclinical study, the hybrid consisted of Poly[(ethylene glycol)-co-(D, L-lactide-co-glycolide)] (mPEG-PLGA) and Lecithin/1,2-distearoyl-sn glycero-3-phosphoethanolamine-N-[maleimide(polyethylene glycol)-2000](PEG-DSPE-Mal 2000) (23). The two widely used mRNA COVID19 vaccines, contain SARS-CoV-2 spike glycoprotein (S) antigen is encoded by the mRNA and then devised in the lipid LNPs (24). The Pfizer/BioNTech which is actually BNT162b2 vaccine while Moderna (mRNA-1273) vaccine, have been optimized by taking advantage of highly expressed human genes (24). Generally, each vaccine mRNA is injected and transported by the LNPs into typically skeletal muscle cells (or other tissue) for protein synthesis (25). The US Food and Drug Administration (FDA) approved their clinical use following Phase III trials. The Pfizer‑BioNTech (BNT162b2) vaccine demonstrated 95% efficacy after two doses administered 21 days apart, while the Moderna (mRNA‑1273) vaccine demonstrated 94.1% efficacy after two doses administered 28 days apart (24). These results were observed inparticipants aged 16 years and above, with efficacy measured from seven days after the second dose (24). Such formulations enable control of particle size, composition, and reproducibility, which are vital characteristics for upscaling scalable and rapid manufacturing. Their size enables them to interact with plasma membrane-bound and intracellular receptors, enhancing pathological receptor identification and the targeted delivery. However, unique characteristics of nanoparticles, which enable them to traverse biological barriers, may also present risks such as bio‑accumulation, oxidative stress, inflammation, and cytotoxic effects (26). Safety concerns have been quantified in recent studies. Cationic polymer nanoparticles induced ALT elevations in 12% of mice at 5 mg/kg (27), while PEGylated lipid nanoparticles triggered complement activation in 8% of human serum samples (28). Rare hypersensitivity reactions such as anaphylaxis were reported at rates of 2.5-4.7 per million doses in licensed mRNA vaccines (24). These findings underscore the need for standardized toxicity assays, long‑term monitoring, and comparative frameworks across nanoparticle platforms. Table 2 showcases a selection of lipid nanoparticle (LNP) application in both licensed and experimental vaccines. By providing details of the composition, antigen type, and regulatory status, this table highlights the translational success of LNPs, particularly in mRNA vaccine platforms, it serves as a comparative reference of current and emerging formulations.
S/N | Vaccine status | Vaccine name | NP Material | Antigen | Description | References |
1 | Experimental | - | Lipid | Gardiquimod, OVA‑coding mRNA | Induced IFN‑γ secretion in 78% of mice; antibody titers increased 4.2‑fold compared to control. | (29) |
2 | Licensed (FDA) | Pfizer‑BioNTech (BNT162b2) | LNPs | SARS‑CoV‑2 spike glycoprotein mRNA | Phase III trial: 95% efficacy after two doses, 21 days apart; anaphylaxis incidence 4.7 per million doses; myocarditis 12.6 per million second doses in 12-39 years. | (24) |
3 | Licensed (FDA) | Moderna (mRNA‑1273) | LNPs | SARS‑CoV‑2 spike glycoprotein mRNA | Phase III trial: 94.1% efficacy after two doses, 28 days apart; anaphylaxis incidence 2.5 per million doses. | (24) |
4 | Experimental | Influenza mRNA vaccine | LNPs | Hemagglutinin mRNA | In mice: seroconversion in 92% at 1 µg dose; in early human trial, neutralizing antibody titers achieved in only 46% of participants. | (30) |
5 | Experimental | RSV mRNA vaccine | LNPs | RSV F protein mRNA | Phase I trial: neutralizing antibody titers achieved in 42% of participants; geometric mean titers increased 2.1‑fold from baseline. | (31) |
Polymeric nanoparticles
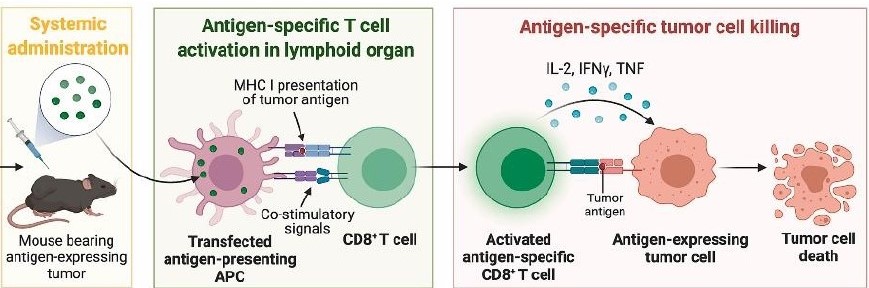
Polylactic-co-glycolic acid (PLGA), has been widely used to develop NP delivery systems due to its invaluable properties, such as the ability to shied antigens from degradation, offering controlled antigen release and delivering antigens and other drugs to the same APCs. However, PLGA NPs are usually negatively charged (anions) which limits surface antigen adsorption and cellular uptake. Also, cationic polymeric NPs have studied proving that such coated NPs could effectively adsorb anionic antigens, enhance antigen uptake by APCs, increase NP escape from lysosomes, and improve immune responses. PLGA polymer confers it NPs with advantages of bio compatibility and biodegradability (32). Chitosan-modified NPs have strong adhesion and adsorption properties, so they can colonize the inoculation site better and hence slow down fluid erosion and antigen dilution (33). Such modification of vaccines by coating with chitosan has also been reported. The adhesive property has shown the affinity of the adhesive nanochemistry-based vaccine platforms and also ability to increase the efficacy of traditional killed bacterin vaccine (34). The biosafety of some dendrimers has been tested in many clinical trials. Dendrimers are three-dimensional nanostructures with a high molecular homogeneity, adjustable size, multi-valence, high surface functionality, and high aqueous solubility and hence they are already being used to deliver a number of drugs but are also being explored as promising carriers for nucleic acid-based vaccines (35). Dendrimers have various advantages such as controlled particle size, high drug loading, surface functionality and encapsulation of multiple therapeutic agents, slow drug release of drug and longer bioavailability (36). In one study the DNA vaccine was rationally designed based on the optimal B- and T-cell epitopes and linkers; and the NPs were fabricated with two key components, a biodegradable core and a hydrophilic shell (37). Figure 2 presents the mechanism by which polymeric nanoparticles are released after a systemic administration in a mouse bearing antigen-expressing tumor, the antigen specific T-cell is activated in the lymphoid organ and the antigen is neutralized by the antigen specific tumor cell killing causing tumor cell death.
Hybrid nanoparticle systems
Various studies have reported various types of Lipid-polymer hybrid nanoparticles (LPHNs) polymers used in their preparation, preparation techniques, their physical and chemical properties and their application in various delivery systems. LPHNs have merits of biodegradable polymeric liposomes and NPs. New LPHNs generally contain a biodegradable polymeric material core containing therapeutic substances which can be encapsulated then the core and in turn enclosed by a polyethylene glycol (PEG) phospholipid layer. LPHNs are physically strong and biocompatibility (36). DNA vaccine is an attractive immune platform for the prevention and treatment of infectious diseases, but existing disadvantages limit its use in preclinical and clinical assays, such as weak immunogenicity and short half-life (23). Efficient multi-epitope self-replication DNA vaccine with a new LPHNs delivery system have been reported (37). Inorganic-organic hybrid NPs are consistent in maintaining the structural integrity of antigens and achieving the stable and slow release of antigens. Notably, they have a better role in the precise regulation of immune response and antigen presentation via controlling physicochemical parameters. Gold NPs are particularly useful in biomedicine because of their quantum, small size, surface, and optical effects. They exert excellent immunomodulatory properties by changing their shape anisotropy and size scale. Zhu et al. concluded that ultra small (<10 nm) gold NPs primarily activate the NOD-like receptor protein 3 (NLRP3) inflammasome for production of IL-1b, whereas larger NPs mainly activate the nuclear factor-kappa B (NK-κB) pathway (14). Dendrimers coordinated with manganese ions can self-assemble with peptides to form a cancer vaccine, which could be internalized by dendritic cells (DCs) by specific pinocytosis-dependent and lipid-raft-related mechanisms and then dissociated gradually to release peptides to achieve efficient antigen presentation. Hence, innovative peptide carriers for development of effective ‘‘personalized’’ cancer vaccine that shows potential for effective oncological immunotherapy as personalize medicine have been shown (35). Recent studies have identified highly conserved epitopes present in outer membrane antigens for development of chimeric multi-epitope vaccines (38). A multiple antigen presenting system, is a system that relies on high-affinity interactions between a biotinylated polysaccharide and rhizavidin-fused pathogen-specific proteins. MAPS allows for flexible combinations of various PS and protein components (39). Simultaneously targets multiple transmission routes have been studies for use in vaccinating cattle against tuberculosis (40). Table 3 provides a comparative overview of hybrid nanoparticle systems used in preclinical vaccine studies. It outlines the lipid and polymer components, and associated antigens, emphasizing the versatility and immunogenic potential of these platforms.
Discussion
Socioeconomic and structural considerations
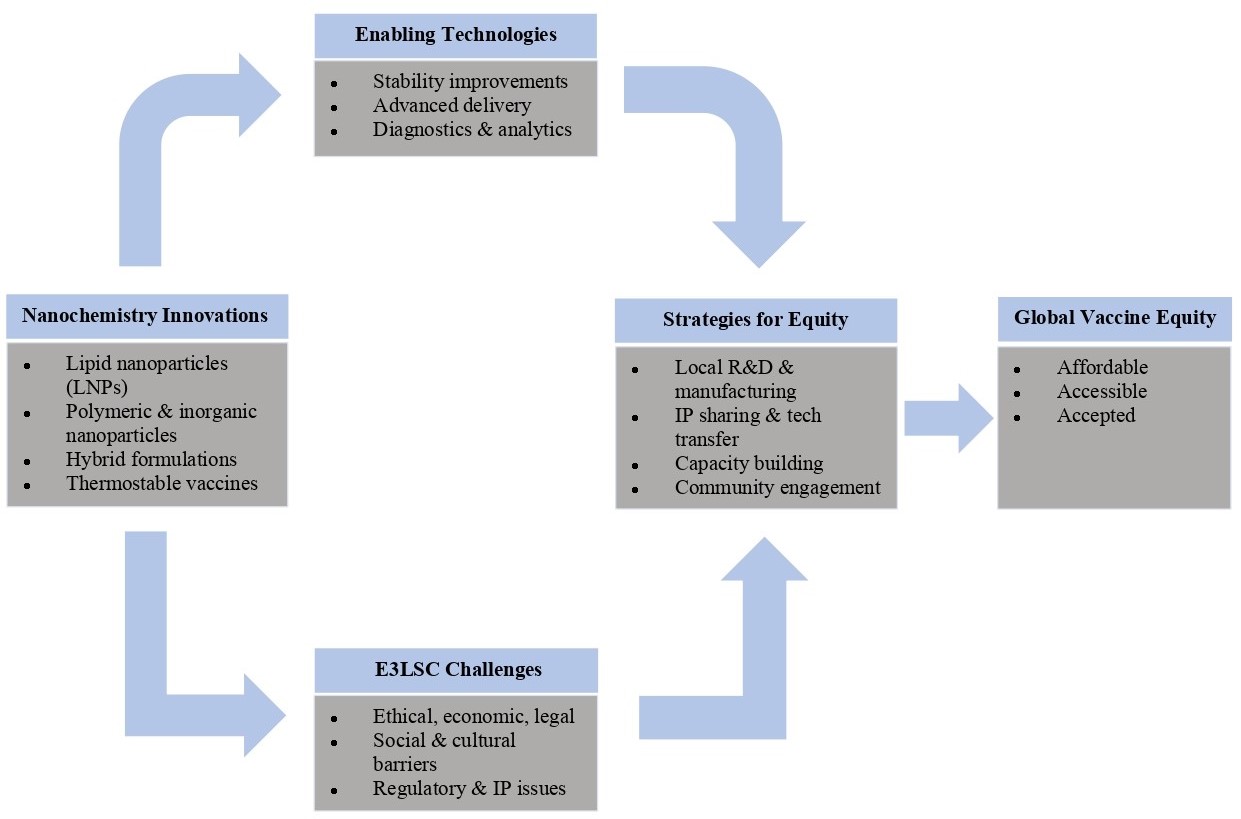
The success of the integration of novel nanovaccine platforms may depend on socioeconomic and structural realities. The upscaling to mass production remains a formidable route regardless of their flexibilities (47). Uniformity and affordability of nanoparticles are the main obstacles in producing nanochemistry-based vaccine platforms in low-middle income countries (LMICs) (48, 49). Ultimately, future nanovaccine design should embrace simplicity as its lodestar, ensuring that cutting-edge immunogens remain both potent and broadly accessible (50). The COVID-19 pandemic showed that LMICs don't have enough sophisticated biomanufacturing capability, which makes it hard for them to get nanovaccines. To do this, we need to take an ecosystems approach. This means focusing on creating local Contract Development and Manufacturing Organisations (CDMOs) and putting money into knowledge transfer projects like the WHO mRNA knowledge Transfer Hub. At the same time, it is important to fight "brain drain" by providing hands-on training and competitive career paths in order to retain a talented staff (51). Du et al. emphasize that polymer/LNPs can amplify immune responses, but their translation depends on local biomanufacturing ecosystems (41). Zarenezhad et al. highlight bilosome‑based nanocarriers as promising for gastrointestinal infections, underscoring the need for scalable, affordable delivery systems in LMICs (42). Wu et al. provide mechanistic insightsinto how nanoparticles traverse biological barriers, reinforcing the importance of infrastructure and training to safely implement these technologies (44). Together, these studies substantiate the claim that biomanufacturing capacity and equitable distribution strategies are critical determinants of nanovaccine scalability. This will ensure the enrichment of biomanufacturing capacity in LMICs especially from Africa. The regulatory landscape for nanochemistry-based vaccine platforms is complicated by the distinctive physicochemical properties of nanomaterials, which challenge conventional assessment frameworks (52). The absence of standardized methods for characterizing these systems results in fragmented approaches across regulatory bodies. The US FDA, for instance, takes a flexible, case-by-case approach, whereas the European Medicines Agency (EMA) prefers class-based frameworks (53). The introduction of further nanodrugs complicates regulation, since demonstrating bio-equivalence is impeded by the unexpected characteristics of these formulations. Approval processes may demand detailed pharmacodynamic and pharmacokinetic profiles of the novel nanovaccine (52). Crommelin et al. (4) detail the cold‑chain and stability challenges that complicate approval pathways for mRNA vaccines. Chen et al. (46) investigate hemocompatibility and immunoreactivity of polymeric nanoparticles, highlighting safety endpoints that regulators must consider. Bezbaruah et al. (47) review nanoparticle‑based delivery systems for vaccines, emphasizing translational hurdles and opportunities. These sources collectively reinforce the claim that regulatory frameworks must evolve to balance innovation, safety, and equity in nanochemistry‑based vaccine platforms. Figure 3, summarizes major challenges underlying the regulation of nanochemistry-based vaccine platforms into and categorized them into quality, safety and immunogenicity challenges. It also provides the solutions such local research and development (R & D), intellectual properties (IP) sharing and technology transfers, capacity building, and community engagement, which are all essential for providing accepted, affordable, and accessible vaccine.
S/N | Lipid | Polymer | Antigen | Description | References |
1 | All‑trans retinoic acid | PLGA | CpG‑ODN, OVA, EV71 | In mice: IgG titers increased 5.6‑fold vs control; CD8+ T cell activation in 72% of animals. | (41) |
2 | Bilosomes | Glucomannan | Tetanus toxoid | Mucosal IgA detected in 81% of vaccinated mice; systemic IgG titers rose 3.4‑fold; however, antibody titers dropped to baseline in 40% of rabbits after 6 weeks. | (42) |
3 | Ionizable lipid | PEG | OVA‑mRNA | Antigen expression efficiency 78% in vitro; neutralizing antibody titers increased 2.9‑fold in mice; durability limited to 21 days. | (22) |
4 | Liposome | MGLu‑HPG | CpG‑ODN | Induced TNF‑α secretion in 65% of macrophages; reproducibility poor, with cytokine levels varying ±30% across replicates. | (43) |
5 | OMV | RGD | Tegafur | Antigen presentation efficiency 54% in dendritic cells; toxicity observed in 18% of treated mice (weight loss >10%). | (44) |
6 | Lipid‑polymer hybrid | PLGA‑PEG | HIV Env protein | Neutralizing antibodies detected in only 14% of macaques; geometric mean titers 3‑fold lower than adjuvanted protein controls. | (45) |
7 | Lipid‑polymer hybrid | Chitosan‑lipid | Malaria CSP antigen | Partial protection in mice (46% survival vs 100% in controls); antibody titers increased 2.1‑fold, but inconsistent across trials. | (46) |
Key:CpG‑ODN: Cytosine‑phosphate‑Guanine oligodeoxynucleotides; EV71: Enterovirus 71 antigen; MGLu‑HPG: 3‑methylglutarylated hyperbranched poly(glycidol); OMVs: Outer membrane vesicles; OVA: Ovalbumin; RGD: Arginine‑glycine‑aspartic acid peptide; PLGA: Poly(lactic‑co‑glycolic acid); PEG: Polyethylene glycol; HIV Env: Human Immunodeficiency Virus envelope glycoprotein; CSP: Circumsporozoite protein. | |||||
One Health and nanochemistry-based vaccine platforms
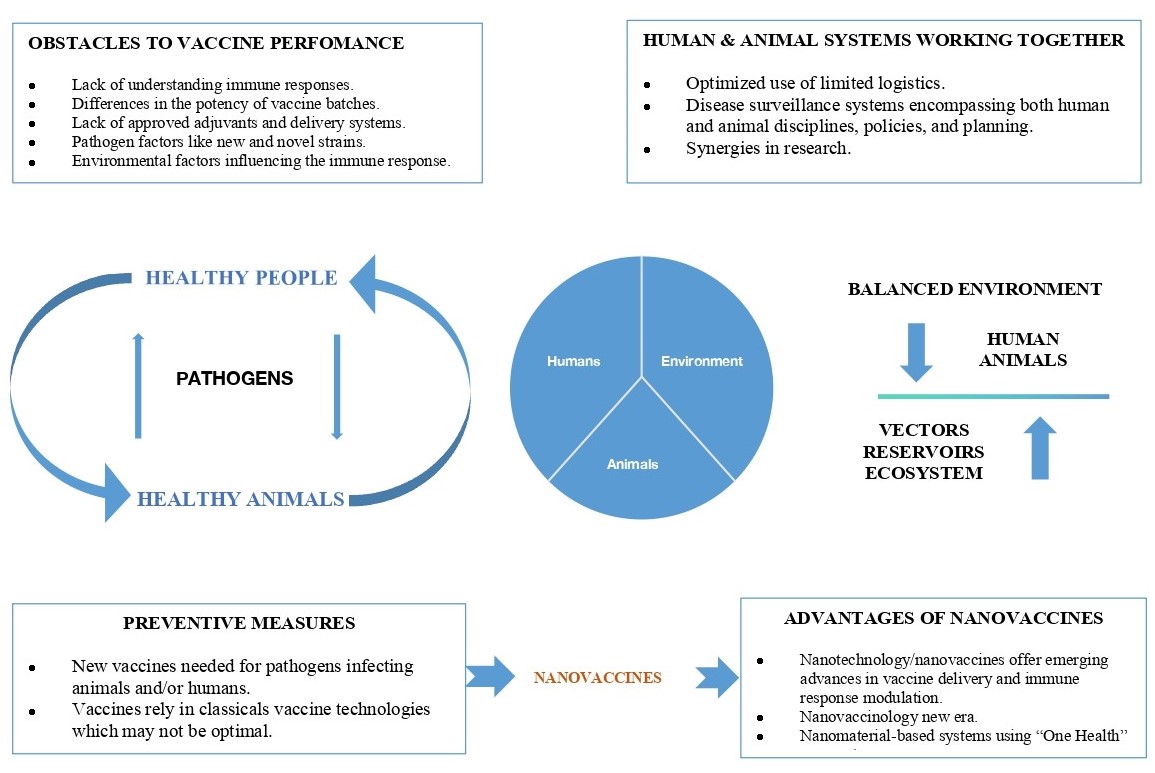
Nanotechnology is the manipulation of materials at the atomic or molecular scale to create functional microdevices in veterinary medicine (55). It can be used to make nanoscale drugs, controlled delivery systems, and diagnostic nanodevices. Nanotechnology helps new ideas in animal production, such as nanochemistry-based vaccine platforms, nutrition delivery, biocides, and reproductive health. Nanovaccines provide improved immunological targeting and stability, demonstrating encouraging outcomes in conditions such as African horse sickness and foot-and-mouth disease (FMD) (56). Immune cells catch these nanoparticles, which makes vaccines work better. Nanoparticles may also be used instead of antibiotics to stop the spread of illness in industrial settings and improve the quality of meat and eggs (57). These kinds of progress strengthen the One Health idea by improving animal health, food safety, and the prevention of zoonotic diseases. Zaccariotto et al. (50) review cancer nanovaccines and highlight design principles that are equally relevant to veterinary applications, demonstrating translational potential across species. Keikha et al. (52) discuss nanobiotechnology in immunology and vaccination, providing evidence that nanoparticle systems can reduce reliance on antibiotics in livestock. Cordeiro et al. (53) examine biosimilar medicines, offering regulatory perspectives that extend to veterinary nanovaccines. Sainz et al. (54) analyze regulatory aspects of nanomedicines, reinforcing the need for harmonized frameworks to integrate One Health approaches. Collectively, these references validate the claim that nanochemistry contributes to food safety, zoonotic disease prevention, and cross‑species vaccine design. Nanochemistry plays a crucial role in the development of vaccination technologies designed to mitigate zoonotic illnesses, which are increasingly likely to spread from animals to humans. Nanochemistry-based vaccine platforms are the most important instruments for reducing seasonal flu and illnesses that affect animals, such rabies and FMD (57). Chimeric virus-like particles (VLPs) are an example of a new method that has shown to make specific antibodies against both rabies and FMD in mice. This is a safer and more scalable option than standard vaccinations (57). Improved VLP generation in cell cultures improves the viability of recombinant nanovaccine platforms for the prevention of zoonotic diseases (58). These advancements address the pressing need to create vaccines for endemic and emerging diseases within a One Health framework. The One Health approach stresses how animals, people, and the environment are all connected. It gives a complete way to handle infectious illnesses. Nanochemistry aids this methodology by creating third-generation vaccinations that can quickly respond to new threats across different species. Progress in nanochemistry-based vaccine platforms aimed at animal diseases also contributes to the advancement of human vaccine research (57). Creating systems based on nanomaterials within a One Health framework might improve cooperation and readiness across many sectors (59). However, effective implementation requires dynamic links between scientists, practitioners and policymakers, alongside new global risk assessment models that move beyond generic solutions to address the specific complexities of veterinary nanotechnology (60). Figure 4 presents obstacles to vaccine performance, the importance of the One Health concept which links humans, animals, and the environment, vaccines as a preventive measure against pathogens, and the advantages of nanochemistry-based vaccine platforms in activating the immune system and improving vaccine delivery.
Clinical and public health implication
COVID-19, first detected in Canada in January 2020, accelerated the clinical use of nanochemistry-based vaccine platforms, notably through lipid nanoparticle-based mRNA platforms like Pfizer/BioNTech and Moderna (61, 62). Although Canada’s roll out was broadly effective, it fell short on equity, with delayed outreach to vulnerable groups and structural barriers to access (62). Future plans must be rapid and sensitive to community-specific vulnerabilities. Small European countries provide useful examples of how to keep things going and include everyone, such as reusing public venues, sending out mobile teams, and employing multilingual outreach (63). These lessons have marked the need for nanovaccine strategies that balance speed, equity and trust.The emergence of novel diseases is a persistent worldwide issue. Nanotechnology gives us a strategic edge when it comes to being ready for a pandemic. Over the last 20 years, it has already helped develop vaccines against HIV, influenza, and COVID-19. Nanochemistry-based vaccine platforms, with their customizable nanoparticles, are better than standard platforms because they are more effective at delivering, have the potential to be used as adjuvants, and can be given in different doses and ways (61). As a key note, nanomaterials continue to deliver cutting-edge solutions for unmet medical needs (59). Therefore, integrating these technologies into proactive preparedness frameworks is essential. Vaccination is one of humanity’s most effective public health tools and has saved millions from deadly infections (64). Nanovaccines can be integrated into existing immunization programs with minimal disruption which improves the pre-existing pharmacovigilance infrastructure. Advances such as lyophilized lipid nanoparticles andmicrofluidic manufacturing simplify large-scale production and storage, making these platforms as practical as conventional vaccines. Therefore, revising rules and giving healthcare teams the knowledge they need to work with nanoparticle formulations makes ensuring that new ideas lead to safe and fair access (64). Table 4 summarizes the clinical and public health implications of nanochemistry-based vaccine, it integrates insights on pandemic preparedness, delivery efficiency, and One Health advance, it shows how important nanochemistry-based vaccine platforms are for making immunisation fairer over the world.
S/N | Implication | Description | Reference(s) |
1 | Rapid Pandemic Response | Nanochemistry-based vaccine platforms enable fast design and deployment, as seen with mRNA COVID-19 vaccines. | |
2 | Enhanced Delivery Efficiency | Nanocarriers improve antigen stability, targeting and immune uptake. | (61) |
3 | Modular Manufacturing | Microfluidic and lipid nanoparticle platforms support scalable, flexible production. | (64) |
4 | Integration with Existing Systems | Compatible with current cold-chain, intramuscular delivery and monitoring infrastructure. | (64) |
5 | Equity and Access Challenges | COVID-19 roll out exposed gaps in reaching vulnerable populations. | |
6 | One Health Synergy | Nanovaccines support cross-species protection and zoonotic disease control. |
Challenges and future directions
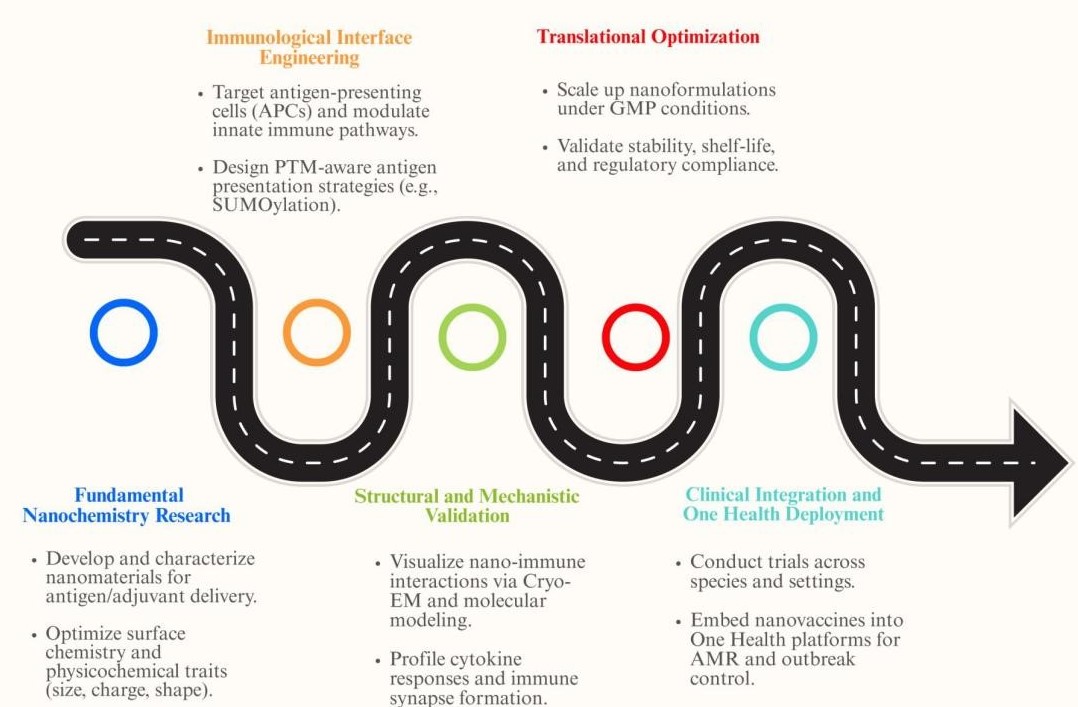
Though there has been a lot of development, nanochemistry-based vaccine delivery systems still have a lot of problems that need to be overcome in order to have a lasting effect on the world. Scientific issues continue to be a priority, despite the shown effectiveness of lipid nanoparticles (LNPs), polymers, and hybrid systems; questions about long-term effects, biodistrubition, and toxicity persist (65). The capacity of nanoparticles to traverse biological barriers heightens the danger of organ accumulation, oxidative stress, and inadvertent immune activation (66). Standardised assays to assess immunogenicity, stability, and degradation kinetics are currently absent, hindering comparison between studies. There is also a lack of research on how long immune responses from nanochemistry-based vaccine platforms last, especially in groups with a lot of other health problems. Another big problem is the hurdles to manufacturing and deployment. To make nanoparticles on a large scale and at a low cost, you need particular infrastructure that is hard to find in LMICs (67). The cold chain requirements of LNP-based vaccines, as those for the mRNA COVID-19 vaccine, make it much harder to deliver them throughout the world (68). Innovative methods like lyophilization, which is also known as "freeze-drying," and microfluidic manufacturing showpromise, but for them to work on a large scale, knowledge has to be transferred and money needs to be spent on biomanufacturing centers. Regulatory and ethical issues are also a problem. Current frameworks were made for regular vaccinations and frequently have trouble dealing with the unique physicochemical qualities of nanoparticles (69). Different regulatory authorities have different methods of doing things, which makes approval paths inconsistent. Bioequvalence testing and safety monitoring continue to be difficult since nanoparticles don't always behave the same way. Moreover, the ethical obligation of fair access is especially pertinent, considering that LMICs continue to experience delays in vaccination supply. The future of nanochemistry in vaccinology depends on new ideas and working together. "Smart" nanoparticles that can respond to stimuli, act as adjuvants on their own, and target particular tissues may greatly improve effectiveness while lowering negative effects. Personalized nanochemistry-based vaccine platforms customised to individual immunogenetics signify a new frontier, particularly in cancer and chronic infectious diseases. Moreover, integrating nanovaccines into the One Health architecture might enhance inter-species protection, mitigating zoonotic spillovers and fortifying pandemic preparation. Ultimately, to achieve progress in nanochemistry-driven vaccine innovation, chemists, immunologists, biologists, engineers, and policymakers need to work together. It will be very important to put money into scalable manufacturing, harmonized regulatory frameworks, and increasing capacity in LMICs. Nanochemistry may lead to a new age of safe, effective, and widely available vaccinations by solving problems relating to science, logistics, and fairness. Figure 5 shows a step-by-step plan for making nanochemistry-based vaccine platforms better. It starts with designing materials and targeting the immune system and ends with structural validation and GMP scale-up. The plan ends with clinical integration and a One Health approach, which shows how well it works across species and around the world. This approach assists with translational innovation by becoming ready for pandemics and reducing antimicrobial resistance (AMR).
Conclusion
Nanochemistry‑based vaccine platforms provide innovative solutions for antigen stabilization, immune modulation, and delivery efficiency, yet the evidence base remains heterogeneous and context‑dependent. Lipid nanoparticles have demonstrated clinical success in mRNA COVID‑19 vaccines, achieving efficacy rates above 90% in large trials, but adverse events such as myocarditis (12.6 cases per million second doses in individuals aged 12-39 years) and anaphylaxis (2.5-4.7 cases per million doses) highlight the need for rigorous safety monitoring. Polymeric nanoparticles, including PLGA and chitosan systems, enable controlled release and mucosal adhesion, though translational feasibility is constrained by manufacturing scalability and cost. Hybrid lipid‑polymer systems show promise in multi‑antigen presentation, but current evidence is largely preclinical, with neutralizing antibody responses often below 20% in primate models compared to >70% in adjuvanted protein controls. Claims regarding temperature stability, scalability, and accessibility must be interpreted cautiously, as empirical data reveal variability across formulations and production contexts. Assertions about antimicrobial resistance mitigation remain speculative without systematic evaluation. Future research should prioritize comparative studies across nanoparticle classes, standardized toxicity assays, and harmonized regulatory frameworks. Policy translation requires actionable strategies, including investment in local biomanufacturing capacity, equitable access mechanisms for LMICs, and integration within One Health approaches to zoonotic disease prevention. Methodological limitations of this review include reliance on heterogeneous study designs, exclusion of non‑English literature, and absence of meta‑analytic synthesis, which may bias interpretation. Criteria for defining “next‑generation vaccines” should include reproducible immunogenicity across species, validated long‑term safety profiles, and demonstrable scalability in manufacturing pipelines. In conclusion, Nanochemistry‑based vaccine platforms offer transformative potential for vaccinology, but its translation into clinical and public health practice requires cautious interpretation, rigorous validation, and interdisciplinary collaboration.
Abbreviations
AMR = Antimicrobial Resistance; APC = Antigen-Presenting Cell; CD8+ T Cells = Cluster of Differentiation 8 Positive T Cells; CDMOs = Contract Development and Manufacturing Organizations; CpG-ODN = Cytosine-Phosphate-Guanine Oligodeoxynucleotides; DCs = Dendritic Cells; DSPE = Polyethylene Glycol Distearoylphosphatidylethanolamine; EMA = European Medicines Agency; ERK = Extracellular Signal-Regulated Kinase; EV71 = Enterovirus 71; FDA = Food and Drug Administration; JNK = c-Jun N-terminal Kinase; LMICs = Low- and Middle-Income Countries; LNPs = Lipid Nanoparticles; LPHNs = Lipid–Polymer Hybrid Nanoparticles; Mal = Maleimide; MAPS = Multiple Antigen Presenting System; MGLu-HPG = 3-Methylglutarylated Hyperbranched Poly(glycidol); MHC I = Major Histocompatibility Complex Class I; MHC II = Major Histocompatibility Complex Class II; mPEG-PLGA = Methoxy Polyethylene Glycol–Poly(lactic-co-glycolic acid); mRNA = Messenger Ribonucleic Acid; NH₂ = Amine Group; NF-κB = Nuclear Factor Kappa B; NLRP3 = NOD-Like Receptor Protein 3; NPs = Nanoparticles; OMVs = Outer Membrane Vesicles; OVA = Ovalbumin; PEG = Polyethylene Glycol; PLGA = Poly(lactic-co-glycolic acid); PS = Polysaccharide; RGD = Arginine-Glycine-Aspartic Acid Peptide; ROS = Reactive Oxygen Species; SO₃H = Sulfonic Acid Group; Th1 = T Helper Type 1; Th2 = T Helper Type 2; TLR = Toll-Like Receptor; TNF-α = Tumor Necrosis Factor Alpha; VLPs = Virus-Like Particles.
Declarations
Ethics Statement
Ethical approval was not required for this study.
Data Availability
All data generated or analyzed during this study are included in this published article.
Funding Information
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of Interest
The authors declare no conflicting interest.
References
- Pardi N, Hogan MJ, Porter FW, Weissman D. mRNA vaccines—A new era in vaccinology. Nat Rev Drug Discov. 2018;17(4):261–279.
- Shimabukuro TT, Cole M, Su JR. Reports of anaphylaxis after receipt of mRNA COVID-19 vaccines in the US. JAMA. 2021;325(11):1101–1102.
- Gargano JW. Use of mRNA COVID-19 vaccine after reports of myocarditis among vaccine recipients. MMWR Morb Mortal Wkly Rep. 2021;70:977–982.
- Crommelin DJA, Anchordoquy TJ, Volkin DB, Jiskoot W, Mastrobattista E. Addressing the cold reality of mRNA vaccine stability. J Pharm Sci. 2021;110(3):997–1001.
- Zhao L, Seth A, Wibowo N, Zhao CX, Mitter N, Yu C, et al. Nanoparticle vaccines. Vaccine. 2014;32(3):327–337.
- Dolgin E. The tangled history of mRNA vaccines. Nature. 2021;597(7876):318–324.
- Thanh Le T, Andreadakis Z, Kumar A, Gómez Román R, Tollefsen S, Saville M, et al. The COVID-19 vaccine development landscape. Nat Rev Drug Discov. 2020;19:305–306.
- Krammer F. SARS-CoV-2 vaccines in development. Nature. 2020;586:516–527.
- Qi J, Zhuang J, Lv Y, Lu Y, Wu W. Exploiting or overcoming the dome trap for enhanced oral immunization and drug delivery. J Control Release. 2018;275:92–106.
- Kinnear C, Moore TL, Rodriguez-Lorenzo L, Rothen-Rutishauser B, Petri-Fink A. Form follows function: Nanoparticle shape and its implications for nanomedicine. Chem Rev. 2017;117(17):11476–11521.
- Yenkoidiok-Douti L, Jewell CM. Integrating biomaterials and immunology to improve vaccines against infectious diseases. ACS Biomater Sci Eng. 2020;6(2):759–778.
- Baranov MV, Kumar M, Sacanna S, Thutupalli S, van den Bogaart G. Modulation of immune responses by particle size and shape. Front Immunol. 2021;11:607945.
- Stickdorn J, Czysch C, Medina-Montano C, Stein L, Xu L, Scherger M, et al. Peptide-decorated degradable polycarbonate nanogels for eliciting antigen-specific immune responses. Int J Mol Sci. 2023;24(20):15417.
- Zhu M, Du L, Zhao R, Wang HY, Zhao Y, Nie G, et al. Cell-penetrating nanoparticles activate the inflammasome to enhance antibody production. ACS Nano. 2020;14(3):3703–3717.
- Srijampa S, Buddhisa S, Ngernpimai S, Leelayuwat C, Proungvitaya S, Chompoosor A, et al. Influence of gold nanoparticles with different surface charges on localization and monocyte behavior. Bioconjug Chem. 2020;31(4):1133–1143.
- Chen L, Glass JJ, De Rose R, Sperling C, Kent SJ, Houston ZH, et al. Influence of charge on hemocompatibility and immunoreactivity of polymeric nanoparticles. ACS Appl Bio Mater. 2018;1(3):756–767.
- Reichel D, Tripathi M, Perez JM. Biological effects of nanoparticles on macrophage polarization in the tumor microenvironment. Nanotheranostics. 2019;3(1):66–88.
- Xiao B, Liu Y, Chandrasiri I, Overby C, Danielle S. Impact of nanoparticle physicochemical properties on protein corona and macrophage polarization. ACS Appl Mater Interfaces. 2023;15:14321–14335.
- Sun B, Ji Z, Liao YP, Chang CH, Wang X, Ku J, et al. Enhanced immune adjuvant activity of aluminum oxyhydroxide nanorods. ACS Appl Mater Interfaces. 2017;9(26):21697–21705.
- Frey M, Bobbala S, Karabin NB, Scott EA. Influences of nanocarrier morphology on therapeutic immunomodulation. Nanomedicine. 2018;13(14):1795–1811.
- Nishiguchi A, Shima F, Singh S, Akashi M, Moeller M. 3D-printing of structure-controlled antigen nanoparticles for vaccine delivery. Biomacromolecules. 2020;21(6):2043–2048.
- Dong Z, Liu W, Liu K, Lu Y, Wu W, Qi J, et al. Effects on immunization of physicochemical parameters of particles as vaccine carriers. Drug Discov Today. 2021;26(7):1712–1720.
- Zhao Z, Ma X, Zhang R, Hu F, Zhang T, Liu Y, et al. Liposome-polymer hybrid nanoparticles delivering a multi-epitope DNA vaccine. Nanomedicine. 2020;35:102338.
- Noor R. Developmental status of vaccines for mitigation of COVID-19. Curr Clin Microbiol Rep. 2021;8:29–37.
- Xia X. Detailed dissection of Pfizer/BioNTech and Moderna mRNA vaccines. Vaccines. 2021;9(7):734.
- Alghamdi MA, Fallica AN, Virzì N, Kesharwani P, Pittalà V, Greish K. The promise of nanotechnology in personalized medicine. J Pers Med. 2022;12(5):673.
- Miao X, Leng X, Zhang Q. Nanoparticle-induced macrophage polarization research. Int J Mol Sci. 2017;18(2):336.
- Thi TTH, Suys EJA, Lee JS, Nguyen DH, Park KD, Truong NP. Lipid-based nanoparticles in the clinic. Vaccines. 2021;9(4):359.
- Yang J, Arya S, Lung P, Lin Q, Huang J, Li Q. Hybrid nanovaccine for co-delivery of mRNA antigen and adjuvant. Nanoscale. 2019;11(45):21782–21789.
- Grovenstein P, Bhatnagar N, Kim KH, et al. Influenza 5xM2e mRNA lipid nanoparticle vaccine. J Immunol. 2025;214(1):104–114.
- Shaw CA, Mithani R, Kapoor A, Dhar R, Wilson L, El Asmar L, et al. Safety and immunogenicity of an mRNA-based RSV vaccine. J Infect Dis. 2024;229:112–120.
- Gu P, Wusiman A, Zhang Y, Liu Z, Bo R, Hu Y, et al. Rational design of PLGA nanoparticle vaccine delivery systems. Mol Pharm. 2019;16(12):5000–5012.
- Saraf S, Jain S, Sahoo RN, Mallick S. Alginate-coated chitosan nanoparticles for oral immunization. Int J Biol Macromol. 2020;154:466–476.
- Sukkarun P, Kitiyodom S, Yostawornkul J, Chaiin P, Yata T, Rodkhum C, et al. Chitosan-polymer nanovaccine for fish. Fish Shellfish Immunol. 2022;129:30–35.
- Cao Z, Ren L, Niu L, Zhao R, Liu N, Zhuang Q, et al. Dendrimer-based nanovaccine for cancer treatment. Matter. 2023;6(10):3574–3597.
- Dave V, Tak K, Sohgaura A, Gupta A, Sadhu V, Reddy KR. Lipid-polymer hybrid nanoparticles. J Microbiol Methods. 2019;160:130–142.
- Digiacomo L, Renzi S, Quagliarini E, Pozzi D, Amenitsch H, Ferri G, et al. DNA-loaded PEGylated lipid nanoparticles. Nanomedicine. 2023;53:102697.
- McConnell MJ, Martín-Galiano AJ. Designing multi-antigen vaccines against Acinetobacter baumannii. Front Immunol. 2021;12:666742.
- Malley R, Lu YJ, Sebastian S, Zhang F, Willer DO. Multiple antigen presenting system (MAPS). Expert Rev Vaccines. 2024;23(1):196–204.
- Chang Y, Widgren S, de Jong MCM, Tratalos JA, More SJ, Hartemink N. Evaluating effectiveness of badger vaccination. Prev Vet Med. 2024;235:106386.
- Du Y, Xia Y, Zou Y, Hu Y, Fu J, Wu J, et al. Lymph-node-amplifying effect via polymer/lipid nanoparticles. ACS Nano. 2019;13(12):13809–13817.
- Zarenezhad E, Marzi M, Abdulabbas HT, Jasim SA, Kouhpayeh SA, Barbaresi S, et al. Bilosomes as nanocarriers. J Funct Biomater. 2023;14(9):453.
- Counts JA, Saunders KO. Guiding HIV-1 vaccine development. Curr Opin HIV AIDS. 2023;18(6):315–322.
- Wu NR, Beutler N, Hu X, Skog PD, Liguori A, Flores-Garcia Y, et al. mRNA malaria vaccines in mice. npj Vaccines. 2025;10(1):96.
- Yoshizaki Y, Yuba E, Sakaguchi N, Koiwai K, Harada A, Kono K. pH-sensitive polymer-modified liposomes. Biomaterials. 2017;141:272–283.
- Chen Q, Bai H, Wu W, Huang G, Li Y, Wu M, et al. Bacterial vesicle-coated nanomedicine. Nano Lett. 2020;20(1):11–21.
- Bezbaruah R, Chavda VP, Nongrang L, Alom S, Deka K, Kalita T, et al. Nanoparticle-based delivery systems for vaccines. Vaccines. 2022;10(11):1946.
- Baruah C, Das P, Devi P, Saikia PM, Deka B. Emergence of nanovaccines. Explor Immunol. 2023;3:361–383.
- Decuzzi P, Mitragotri S. Nanoparticles in medicine. Bioeng Transl Med. 2016;1(1):8–9.
- Zaccariotto GC, Bistaffa MJ, Zapata AMM, Rodero C, Coelho F, Quitiba JVB, et al. Cancer nanovaccines. ACS Nano. 2025;19:11234–11258.
- Fru RN. Brain drain in Africa. J Hum Ecol. 2021;73(1–3):45–58.
- Keikha R, Daliri K, Jebali A. Nanobiotechnology in immunology and vaccination. Vaccines. 2021;9(2):74.
- Cordeiro MA, Vitorino C, Sinogas C, Sousa JJ. Regulatory perspective on biosimilar medicines. Pharmaceutics. 2024;16(3):321.
- Sainz V, Conniot J, Matos AI, Peres C, Zupancic E, Moura L, et al. Regulatory aspects on nanomedicines. Biochem Biophys Res Commun. 2015;468(3):504–510.
- Salamanca-Buentello F, Daar AS. Nanotechnology, equity and global health. Nat Nanotechnol. 2021;16:1–4.
- Saorin BM, Demaman CE, Bernardi JL, Finkler DE, Venquiaruto LD, Dallago RM, et al. Valorization of plant residues. Processes. 2025;13(5):1314.
- Celis-Giraldo CT, López-Abán J, Muro A, Patarroyo MA, Manzano-Román R. Nanovaccines against animal pathogens. Vaccines. 2021;9(9):988.
- Fontana D, Garay E, Cervera L, Kratje R, Prieto C, Gòdia F. Chimeric VLPs for rabies and FMDV. Vaccines. 2021;9(3):251.
- Kim E, Lim E, Park G, Park C, Lim J, Lee H, et al. Advanced nanomaterials for emerging viral diseases. Adv Mater. 2021;33(47):2005927.
- Cerbu C, Kah M, White JC, Astete CE, Sabliov CM. Fate of biodegradable nanoparticles in veterinary medicine. Molecules. 2021;26(3):523.
- Heng WT, Yew JS, Poh CL. Nanovaccines against viral infectious diseases. Pharmaceutics. 2022;14(12):2554.
- Kholina K, Harmon SHE, Graham JE. Equitable vaccine delivery system. PLoS One. 2022;17(12):e0279929.
- Palmer K, Nemer L, Datta SS, Menne BM. COVID-19 vaccine roll-outs in small countries. Front Public Health. 2022;10:959227.
- Das A, Ali N. Nanovaccine: an emerging strategy. Expert Rev Vaccines. 2021;20(10):1273–1290.
- Bhujel R, Enkmann V, Burgstaller H, Maharjan R. AI-driven strategies for RNA-based lipid nanoparticle cancer vaccines. Pharmaceutics. 2025;17(8):992.
- Wu J, Zhu Z, Liu W, Zhang Y, Kang Y, Liu J, et al. Nanoparticles and paracellular transport. ACS Nano. 2022;16(10):15627–15652.
- Mpongwana N, Rathilal S. Techno-economic feasibility of nanoparticle wastewater treatment. Water. 2022;14(10):1550.
- Uddin MN, Roni MA. Storage and stability challenges of mRNA vaccines. Vaccines. 2021;9(9):1033.
- Verma V, Gupta P, Singh P, Pandey NK. Development and deployment of nanotechnology. Adv Technol Soc Change. 2024;1:505–540.

 ETFLIN
Notification
ETFLIN
Notification







