Novasome: Combining Ufasome and Niosome for Excellent Vesicular Drug Delivery System
by Ajeng illastria Rosalina , Erny Sagita , Iskandarsyah Iskandarsyah ★
Academic editor: Abd. Kakhar Umar
Sciences of Pharmacy 2(1): 26-36 (2023); https://doi.org/10.58920/sciphar02010035
This article is licensed under the Creative Commons Attribution (CC BY) 4.0 International License.
22 Feb 2023
06 Mar 2023
06 Mar 2023
09 Mar 2023
Abstract: Novasome technology is a novel encapsulation-based drug delivery method that is more effective and efficient than standard liposome systems. It is composed of a mixture of surfactant, cholesterol, and free fatty acids, which produce superior vesicle characteristics for drug delivery. Various studies have investigated the optimal combination of surfactant type, free fatty acid type, and their ratio, as well as the formulation factors that can significantly affect the vesicle characteristics. The novasome technology has demonstrated its potential for delivering a range of substances, including terconazole, fenticonazole, zolmitriptan, and vaccines. Novasomes can be produced using various methods, such as the thin film hydration (TFH) method, injection method, and vortex method combined with a suitable size reduction method. Future research can focus on exploring the potential of novasome technology for delivering a wider range of drugs and vaccines and developing more efficient and effective methods for producing novasome vesicles.
Keywords: NovasomeLipid vesicleDrug delivery systemDrug carrier
Introduction
Scientists keep exploring new strategies for increasing substance absorption through the skin (1), such as active (microneedles and electric-based enhancers) and passive (penetration enhancers and carriers) techniques (2). The vesicular drug encapsulating system is a carrier method to facilitate skin penetration (3). Drug carriers work on targeted delivery (to an organ, tissue, etc.) and modify drug disposition when used with medications having a pharmacokinetic profile. Vesicular systems have become useful for delivering the payload to specific sites and improving outcomes. Lipid vesicles have applications in immunology, membrane biology, diagnostics and genetic engineering research. Vesicles can also be used in modeling biological membranes and for the transport and targeting of API (4).
The first generation of vesicle technology is a conventional liposome (CLs). It can encapsulate lipophilic or hydrophilic drugs and facilitate skin permeation. However, there’s evidence that it is difficult for CLs to penetrate the deeper layer of the skin (3) due to their confinement and reduced ability to increase systemic drug absorption. Besides that, it has poor encapsulation capacity and drug leakage (2). Scientists have already found new vesicular technology to improve CLs capabilities, such as niosome, transfersome, ethosome, fitosome, ufasome, and novasome, that have their advantages and limitations (1). Novasome technology is a novel encapsulation-based delivery method that is more effective and efficient than standard liposome systems (5). Novasome is a multi-bilayer vesicle with a high nuclear capacity within a narrow size range, allowing it to transport vast quantities of active chemicals (6). The novasome comprises paucillamellar vesicles with a 200–700 nm diameter, constructed of 2–7 bilayer membranes, each containing an amorphous nucleus and an amphiphile molecule. Novasome is regarded as one of the most successful treatments for skin disorders, has nearly no side effects, and does not induce cytotoxicity (7).
Novasome enhances the structure of CLs, ufasome, and niosomes, often composed of cholesterol, free fatty acids, and polyoxyethylene fatty acids (5). This combination is comparable to a mixture of ufasomes containing free fatty acids and niosomes containing a nonionic surfactant. This combination produces a superior drug delivery system with superior properties. Several studies have been carried out to investigate its characteristic. In 1996, Gupta et al. and in 2004, Chambers et al. used novasome as a vaccine adjuvant (6, 8). Abd-Elal et al. (2016) successfully encapsulated zolmitriptan in novasome, and Mosallam et al. (2021) encapsulated terconazole in novasome and proved its superiority compared to niosome (9, 10). Another study by Albash et al. proved that novasome has excellent characteristics in encapsulating fenticonazole nitrate and showed high antifungal potential (11). This review discussed recent novasome research combining ufasome (fatty acid vesicle) and niosome (surfactant vesicle) composition, eventually making better vesicles for drug delivery. Design and production of novasome as drug-delivery devices are described in this article. The study also examines the characteristics to emphasize how novasome are tuneable as drug carriers.
Niosome
Niosomes are vesicular systems made primarily of nonionic surfactants and cholesterol bilayers, similar to liposomes. They can enhance drug efficacy relative to free drugs. Compared to liposomes, these vesicular systems provide advantageous qualities, including excellent chemical stability, cheap cost, simple handling and storage and easy sterilization (12). Surfactants utilized in niosome preparation are biodegradable, non-immunogenic, and biocompatible. As a result of these characteristics, niosomes have attracted increased interest as desirable colloidal carriers (13).
According to reports, niosomes are the most beneficial and successful targeted drug delivery. They are a brand-new method of medication delivery in which the medicine is enclosed in vesicles that self-assemble. In that they consist of a bilayer, they are comparable to liposomes. In contrast to liposomes, where phospholipids make up the bilayer, niosomes have a nonionic surfactant. Depending on the type of preparation used to produce them, niosomes can be either uni- or multilamellar. Although niosomes and liposomes have comparable structural features, niosomes have been regarded as a potential alternative drug delivery system because of their capacity to encapsulate a variety of medicines within their multi-environmental structural makeup. (14).
Niosome Composition
Niosome-manufacturing surfactants must have a hydrophilic or polar head and a lipophilic or hydrophobic tail. Typically, the hydrophobic tail comprises one or two alkyl or perfluoroalkyl functional groups or a single steroidal group [20]. Chemically, ester-containing surfactants are less stable than ether-containing surfactants. Ether-containing surfactants are more hazardous because esterase enzymes degrade ester-linked surfactants to produce triglycerides and fatty acids in vivo (15). Surfactants with alkyl chain lengths between C12 and C18 are appropriate for niosome synthesis (16). The HLB value of a surfactant can indicate the material's ability to form a vesicle. Without lipids, surfactants such as Tween® 20, 60, and 80 with HLB values between 14 and 17 cannot form vesicles. However, surfactants such as Span® with an HLB value of 8 can form vesicles (17, 18). It has been proven that the choice of surfactant directly affects the PS, PDI, and, to a lesser extent, the ZP. Larger HLB surfactants typically exhibit a PS accompanied by a greater PDI. (4).
Ufasome
The amphiphilic compounds that have a chain of carbon atoms serving as a nonpolar portion and a terminal carboxylic group functioning as a polar part are how fatty acids are typically described (19). Free fatty acids act as penetration enhancers for the bioactive through the stratum corneum (20). Fatty acid vesicles can effectively carry different enzymes, medications, or other macromolecules because they penetrate hydrophobic layers like skin (19). Fatty acids could form vesicles that can encapsulate bioactive known as ufasomes. Unsaturated fatty acids tend to form vesicles in the aqueous environment. In addition, saturated fatty acids with 8–12 carbon atoms were also found capable of forming vesicles in a pH-dependent manner (21).
Fatty acid vesicles have several interesting characteristics, one of which is their dynamic nature because they are made of single-chain amphiphiles. Dynamic characteristics put fatty acid vesicles between micelles made of single-chain surfactants and ordinary vesicles made of double-chain amphiphiles (22). Although encapsulation yields are sometimes somewhat low, encapsulation of water-soluble compounds within fatty acid vesicles offers a means to localize species. When making fatty acid vesicles, both macromolecules like RNA and small compounds like dyes can be directly enclosed (23) Besides these advantages, these supramolecular aggregates easily undergo oxidation (24), permeable and less stable than standard phospholipid liposomes (25). This lack of stability can be overcome by combining with amphiphilic compounds or other surfactants (25). A novasome combines free fatty acid with a surfactant to fix the limitation.
Ufasome Composition
Fatty acid vesicles known as ufasomes are closed lipid bilayered suspensions comprised of unsaturated fats and their ionized species (soap), with a pH range of 7 to 9. Fatty acid vesicles typically include two forms of amphiphiles, one of which is an ionized form (negatively charged soap), and the other is a nonionic neutral form. The main factors affecting vesicle stability are nonionic neutral and ionic form ratios. Gebicki and Hicks first described the creation of fatty acid vesicles in 1973; oleic and linoleic acids were added to the list in the following years. The vesicles were initially referred to as ufasomes. But later research revealed that in addition to unsaturated fatty acids, saturated fatty acids that resemble octanoic and decanoic acids also produce fatty acid vesicles (26).
Studies on fatty acid surface film analyses show that 12 to 22-carbon fatty acids will be suitable for creating stable ufasomes. Studies were extremely limited because early testing on C-18 fatty acids showed that they provided the highest assurance. Only membranes produced from oleic (cis-9-octadecenoic acid) and linoleic (cis, cis-9, 12-octadecadienoic acid) unsaturated fatty acids are preferred in the creation of ufasomes. On charging the membrane with a small amount of oleic, linoleic, and stearic acid, the ufasome preparation does not improve. Oleic acid has a minimum of six weeks before becoming contaminated, but major peroxides only appear two to three weeks later and are determined by stability tests (26).
Novasome
Novasome is a penetration-enhancing technology with an encapsulation process to deliver various substances effectively. Novavax originally developed this technology. IGI Laboratories, Inc. has a 10-year exclusive license from Novavax for technologies related to most non-pharmaceutical applications (9). Novasomes are modified forms of liposomes or variations of niosomes and ufasome prepared from a mixture of polyoxyethylene fatty acid monoesters, cholesterol and free fatty acids at a ratio of 74:22:4. The basic composition of the novasome and another lipid vesicle is shown in Table 1. The composition forms non-phospholipid paucilamellar vesicles with a diameter of 0.1-1.0 microns consisting of two to seven bilayered shells surrounding a large amorphous core that is either hydrophilic or hydrophobic (5).
Table 1. Comparison of the components of novasome and several other vesicle systems.
|
Komponen |
Liposome |
Niosome |
Ufasome |
Novasome |
|
Phospholipid |
+ |
- |
- |
- |
|
Surfactant |
- |
+ |
+ |
+ |
|
Cholesterol |
+ |
- |
- |
+ |
|
Free Fatty acid |
- |
- |
+ |
+ |
Novasome offers several advantages, such as delivering hydrophilic or hydrophobic ingredients or a combination in the same formulation. Possible interacting drugs may be combined between bilayers to prevent incompatibility. Due to its surface charge characteristics, they can release the drug at a specific location. They can deliver large amounts of active ingredients because it has an adsorption efficiency of 80%, thereby reducing the frequency of administration. It can adhere to the skin or hair shaft, thus offering the added advantage of being used in various cosmetic formulations (5).
Novasome has demonstrated its function as an innovative system for the topical delivery of terconazole to treat fungal skin infections. Terconazole in novasome has the characteristics of small particle size, round morphology, and high adsorption percentage. Microbiological assessment of terconazole in novasome demonstrated its potential efficacy against Candida albicans relative to terconazole suspension. Due to its highly elastic nature, it also exhibits superior deposition in the skin compared to traditional niosomal formulations and terconazole suspensions. In addition, the terconazole in novasome confirms its dermatological safety when applied to the skin. Furthermore, clinical trials proved the superiority of terconazole in novasome compared to placebo in providing a complete clinical cure for Candida albicans infection (10). Albash et al. have also proven to increase the antifungal potency of fenticonazole Nitrate formulated in Trans-Novasome (11).
In addition to increasing penetration in topical preparations, novasome has also been shown to increase targeting to the brain via intranasal preparations. Novasome has been proven successful in encapsulating the hydrophilic drug zolmitriptan, with a high percentage of nanoparticle size. The zolmitriptan preparation in novasome exhibits increased targeting to the brain via the nose compared to the injection solution of zolmitriptan. Thus, zolmitriptan can be developed in a novasome given via the nasal route to treat acute migraine attacks (9). Novasome has also been investigated for use as a carrier for thyroid hormone administered topically to accelerate wound healing in rats (27).
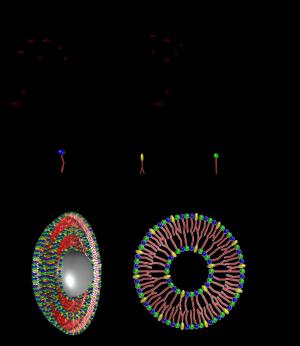
Apart from being used as a carrier vesicle, novasome is also a vaccine adjuvant. Pushko et al. in their research proved that the use of novasome adjuvant on the H9N2 virus antigen could increase the immunogenicity and protection by recombinant vaccines produced by baculovirus-based virus-like particles (VLP) as well as H9N2 VLP and recombinant HA (rH9) vaccines. Therefore, the use of novasome adjuvant needs to be studied further as a potential vaccine component or antigen-sparing agent (28). Molecular structure of novasome is shown in Figure 1.
Advantages of Novasome Compared to Niosome and Ufasome
Novasome offers advantages compared to niosome and ufasome. Mosallam et al. demonstrated the superior effect of novasome compared to niosome. Their research found that novasome has a higher deformability index and better drug deposition inside the skin than niosomal formulation (10). Novasome also has good stability. It can preserve its characteristic better than ufasome. Novasome is stable during 90 days of storage at 25ᵒC and 4ᵒC (10). In contrast, ufasome showed decreased drug content and entrapment efficiency while stored at room temperature (29). Mittal et al. (2013) investigated the stability of dexamethasone-loaded ufasomes stored at room temperature for 30 days, and they observed a rise in particle size and a decrease in entrapment efficiency (30). In addition, Walde et al. stated that ufasome is stable (above the transition temperature/Tc) only within a limited intermediate pH range (19, 31).
Novasome Composition
The main component of novasome is polyoxyethylene fatty acid monoesters, cholesterol and free fatty acids. That composition could vary in type and concentration. Several studies have been carried out recently to investigate the different compositions of novasome shown in Table 2.

Figure 1. Novasome structure in 3D and 2D shapes composed of free fatty acid, cholesterol, and surfactant.
Cholesterol
Cholesterol can modify the fluidity, flexibility, and permeability of membranes in vesicles made from lipids. It essentially fills up the spaces left by other lipid species' shoddy packing (22). Changes in cholesterol concentration seem to have more impact on particle size than changes in surfactant (32). The cholesterol vesicle system helps form a bilayer arrangement and increases rigidity, strength, retention and adsorption efficiency. Physically, the cholesterol molecule will position itself together with the nonionic surfactant on the vesicle membrane (33).
Table 2. Research of finding optimum novasome formula.
|
API |
Vesicle composition |
Method Preparation |
Reference |
|
Tetanus Toxoid vaccice |
Dioxyetylene cetyl ether:oleic acid:cholesterol |
Ethanol injection |
(8) |
|
Fenticonazole |
Span 60:oleic acid:Brij 93/Brij 58:cholesterol |
Ethanol injection |
(11) |
|
Zolmitriptan |
Oleic acid/stearic acid:span 80/span 60:cholesterol |
Thin film hydration |
(9) |
|
Terconazole |
Oleic acid/stearic acid:span 80/span 60:cholesterol |
Ethanol injection |
(10) |
|
Oxiconazole |
Oleic acid:tween:cholesterol |
Vortex |
(34) |
Karal et al. found that increasing cholesterol content may increase the population's large GUV fraction. On the one hand, the theory developed by the Helmholtz free energy framework of the system illustrates satisfactory experimental results. On the other hand, it provides an opportunity to estimate cholesterol's influence on lipid membranes' flexural modulus (35). The molar ratio of cholesterol to Span can influence drug adsorption into vesicles (36). In their research, Abd-Elal., et al. optimized the formula. They obtained the optimal formula for novasome with the ratio of surfactant: fatty acid: cholesterol (1:1:1) (23). In contrast, Mosallam et al., in their research, obtained the optimal formula for the weight ratio of surfactant: fatty acid: cholesterol (5:2:3) (10). Mustafa's research (2015) conducted adsorption and particle size tests of several vesicles by varying cholesterol levels, and the optimal concentration results were obtained by combining the molar ratio of surfactant and cholesterol (5:1) (33). In addition, in another study, acyclovir was well encapsulated in niosomes prepared using cholesterol: Span 80 ratio with a ratio of 1:3 (36).
Surfactant
Nonionic surfactants can affect the lipid bilayer in several ways. The n-alkyl PEO polymer (nonionic surfactant) causes some modification of the bilayer. The molar ratio of the polymeric surfactant can decrease the thickness of the bilayer and gradually change the system to a different micellar structure (37). Surfactant type is known to significantly affect vesicle characteristics such as ZP, PS, PDI and %EE. Mosallam et al. proved using span 60 and 80 for varying surfactant type for novasome formulation. In that research, they found that surfactant type significantly affects ZP. Span 80 gained a greater vesicular bilayer charge than Span 60. This may be due to the more hydrophilic character of Span 60 (HLB 4.7) than Span 80 (HLB 4.3), which may have contributed to the shielding of the (-ve) charge by residing on the surface of the vesicular bilayer. This has resulted in a considerable decline in the ZP value (10).
However, that outcome was different from Abd-Elal et al. founding. They found that the ZP values of Span 60-containing vesicles were substantially greater than those of Span 80-containing vesicles (9). This result agrees with Lingan et al., and they explained that it could be related to the lipophilicity of the surfactant that forms vesicles. Due to the decrease in the surfactant's surface free energy, decreasing the surfactant's lipophilicity increases ZP values. Span 60 (HLB = 4.7) is less lipophilic than 80 (HLB = 4.3). Hence it demonstrated greater ZP values than Span 80 (38). Nonionic surfactants' hydrophilic/lipophilic balance (HLB) reflects the weight distribution of hydrophilic and lipophilic groups within a molecule (39).
In another research, Albash et al. found that Brij 93 had a higher negative ZP value when compared to Brij 58 (11). This may be explained by the fact that Brij 58 is more hydrophilic than Brij 93, which may cause the negative charge to be shielded by clinging to the surface of the novasome bilayers and masking its charge (40). In addition, Brij 93 contained 2 PEG units, and Brij 58 had 20 PEG units, respectively, as was already mentioned. Lower ZP results from the surface charge of TNs being slightly filtered by the increased hydrophilic PEG steric shield concentration.
Surfactant has a substantial effect on the %EE. %EE of vesicles carrying Span 60 is much higher than those having Span 80. This could be attributable to the Span 60's solid composition, hydrophobicity, and phase transition temperature (Tc). Span 60 has a larger Tc (53ᵒC) than Span 80 (-12ᵒC), resulting in greater drug entrapment (9). The degree of saturation of the alkyl chain length is another factor. Even though both surfactants have the same alkyl chain length (C18) (41), the oleate moiety of Span 80 contains a double bond (with comparatively high electron density) at C9, which repels the neighbouring hydrocarbon chains, causing the characteristic 'kink' in the structure (42). This makes the membrane more permeable, which explains why novasomes containing Span 80 had a lower %EE than those having Span 60. The same result was found by Al-Mahallawi et al. about the preparation of tenoxicam-loaded bilosomes. They discovered that the %EE of Span 60 containing vesicles was much greater than that of Span 20 containing vesicles. They linked this to the maximum saturation of the alkyl chain length and Tc and Span 60, which impacted the %EE in the manufactured bilosomes (43). Albash et al., in their research, also found that surfactants had a significant effect on %EE. The difference in HLB values between Brij 93 (HLB=4) and Brij 58 (HLB=15.7) may explain why novasomes containing Brij 93 have greater %EE values (11).
Novasomes PS impacted by surfactant type. Abdel et al. showed that vesicles carrying Span 60 had substantially larger particles than those containing Span 80 (9). Increasing the surface free energy of the surfactant monomers (decreasing lipophilicity) causes the production of bigger vesicles. HLB is higher in Span 60 (4.7) than in Span 80 (4.3) (38). Albash et al. have already shown that Brij type affects vesicle PS, Brij 93 producing a greater PS than Brij 58. This could be associated with the PEG content of the two edge activators, as Brij 93 had 2 PEG units, and Brij 58 included 20 PEG units. It was hypothesized that decreasing the PEG content of the PEGylated edge activator could increase the vesicle precipitation and agglomeration rate, producing a bigger PS (11).
There was a relationship between the vesicle particle size and the drug %EE, with the bigger particle size novasomes having a higher %EE (9). This may be explained by the increase in layer separation, which improves medication incorporation in the hydrophobic region of the vesicles (4). Al-Mahallawi et al., that prepare tenoxicam-loaded bilosomes yielded similar outcomes (43).
Surfactant type had a substantial effect on the dispersion of PDI novasomes as well. Compared to Span 60-containing vesicles, Span 80 contains vesicles exhibiting much lower PDI and greater homogeneity. This may result from their smaller particle size than novasomes made using Span 60 (9).
Free fatty acid
Gupta et al. use oleic acid as FA to create novasome combined with oxyethylene cetyl ether and cholesterol (oxyethylene cetyl ether:cholesterol:oleic acid at a molar ratio of (33:11:7) (8). Mosallam et al. used OA and SA for varying FA types for novasome formulation. In that research, they found that FA type significantly influenced PS and PDI. The stearic acid-formulated novasomes were larger in particle size than those made with oleic acid. This could be explained by the difference in FA melting point, with stearic acid having a melting point of 69°C and oleic acid having a melting temperature of 13°C. A high FA melting point led to an increase in melting viscosity and, thus, a decrease in the efficacy of the sonication stage in PS reduction. Oleic acid-forming vesicles had a substantially lower PDI and better homogeneity than stearic acid-forming vesicles. This could be explained by the decreased PS produced by oleic acid vesicles (10). These findings were consistent with Abd-Elal et al., who examined zolmitriptan-loaded novasomes (9).
According to Mosallam et al., the presence of FA on the surface of vesicles gives novasomes a highly negative charge surface. Oleic acid molecules have a carboxylic group that can be ionizable (10). As a result, it is regarded as an independent ionic lipid. Similar findings were made by Manconi et al., who discovered that using oleic acid during the creation of vesicles resulted in the highest negative charge in vesicles (44).
FA type also significantly affects the %EE of novasome. This may be associated with the saturation level of the alkyl of The chain of the FA. Stearic and oleic acids have identical alkyl chain lengths (C-18). Nevertheless, oleic acid has an unsaturated double bond in its alkyl chain, resulting in a lower Tc than stearic acid (69°C). Oleic acid has a lower Tc (13°C), resulting in more leaky vesicles and reduced entrapment (9). However, Mosallam et al., found different results, and FA type did not significantly affect %EE (10).
Ingredient ratio/concentration
Surfactant quantity considerably influenced the novasome PS. Novasome PS rose with increasing surfactant quantity. This agreed with the %EE results since Span 60 exhibited high %EE levels at high concentrations. The increased drug concentration within the vesicles could cause the bilayer gaps to expand, leading to an increase in PS. In addition, the alkyl chain length of the surfactant may result in a bigger core space and wider vesicle diameter (11). The ratio of Surfactant to FA was discovered to influence the PS. The particle size (PS) of the vesicles increased as the surfactant to free fatty acid (FA) ratio changed from 1:1 to 2:1, which is likely due to the previously mentioned correlation between vesicle PS and encapsulation efficiency (%EE) increase. The increased amount of drug contained within the vesicles' hydrophobic region may have contributed to expanding the space between the bilayers and the subsequent increase in PS (10). In addition, Zaki et al., who worked with diacerein-loaded niosomes, also observed an increase in PS with increasing Span 60 concentration (45). Moasallam also found that the total lipid concentration had a synergistic effect on the PS. This could be due to a large quantity of film-forming components relative to the hydration medium, resulting in the buildup of several layers on top of one another and a consequent rise in PS. In addition, a significant number of lipid components led to a rise in the number of lipid particles in each vesicle, establishing a linear relationship with the vesicle scale. Furthermore, the increase in lipid concentration may have contributed to vesicle heterogeneity and the rise in PDI (10).
Albash et al. found that a rise in FA content increased PS PDI. This could be explained by the fact that the PS and PDI were discovered to be directly correlated, with the novasome with the highest PDI value having the highest PS (11). Owing to the attractive steric interactions, an increase in the chain length of FA decreases the capacity of oil molecules to permeate the interfacial film, resulting in the formation of bigger particles (46). Additionally, oleic acid's angular shape may result in bigger particles. This result was consistent with the earlier discovery by Kumar et al. (2018) using oleic acid vesicles loaded with minoxidil (47).
Increasing oleic acid concentration decreased the %EE. Kumar et al. observed that increasing the amount of oleic acid decreased the %EE of minoxidil. This could be due to an excess of FA, which causes the lipid matrix of a vesicle to degrade, resulting in a decrease in %EE (47). Surfactant to fatty acid ratio also had a significant impact on %EE. It was found that the %EE value increases upon increasing the surfactant to FA ratio from 1:1 to 2:1, which could be attributed to the added emulsification and stabilization impact of the lipid material in the presence of high surfactant concentration. Albash et al. suggested that the %EE value grew as the surfactant quantity increased. This could be attributed to the increased emulsification ability resulting from novasome high surfactant content (11).
Finding the optimum formula for creating the best vesicle characteristic is crucial. Abd-Elal et al. obtained the optimal formula for novasome with a ratio of surfactant: fatty acid: cholesterol (1:1:1) (9). In contrast, Mossalam obtained the optimal formula for the weight ratio of surfactant: fatty acid: cholesterol (5:2:3) (10).
Component interaction
A significant interaction was identified between surfactant type and the type of FA on the %EE. In the presence of oleic acid, the %EE of Span 80-containing vesicles was substantially lower than in the presence of stearic acid. This may be due to the unsaturation in the alkyl chain of both oleic acid and Span 80, which synergistically creates more permeable and leaky vesicles. This causes the drug to escape outside of the vesicles, hence decreasing the %EE. A significant impact of the FA:surfactant ratio was also found. By increasing the molar ratio of FA from 1:1 to 2:1, the %EE of drug-loaded novasomes decreased significantly. This may be ascribed to the likely presence of mixed micelles in the dispersion media, which enhances drug solubility in the dispersion medium when FA concentration increases, hence decreasing the %EE (9).
A substantial interaction was identified between the surfactant type and the FFA to SAA ratio. The particle size of Span 60-containing vesicles reduced dramatically when the ratio of oleic acid to SAA increased from 1:1 to 2:1. By raising the ratio of oleic acid: SAA from 1:1 to 2:1, the particle size of Span 80-containing vesicles was seen to shrink somewhat. To indicate the consistency of vesicle size within the formulation, the PDI was used to measure the particle size distribution width. PDI is the ratio between the standard deviation and the average droplet size (9). A low PDI value indicates a homogeneous monodisperse size distribution, whereas a high PDI value indicates a more heterogeneous polydisperse size distribution (48).
There was a significant interaction between the surfactant type and FA type. Shifting the FA from oleic acid to stearic acid led to considerably lower ZP values of Span 60 vesicles than Span 80 novasomes. Additionally, increasing the oleic acid to surfactant ratio from 1:1 to 2:1 significantly increased ZP (9). Manca et al. got comparable outcomes in their investigation on synthesising rifampicin liposomes (Manca et al., 2012). In contrast, increasing the stearic acid ratio from 1 to 2 decreased the ZP of novasomes (9).
Solvent
The solvent used is dichloromethane because this solvent can dissolve surfactants and fatty acids and is easily evaporated. In their research Abd-Elal., et al. used chloroform as a solvent in the manufacture of novasome (9). Still, in this study, dichloromethane was used because it has a lower boiling point than chloroform (40ᵒC for dichloromethane and 61ᵒC for chloroform), so it is suitable for encapsulation of placenta extract, which is thermolabile. Dichloromethane can also be removed by evaporation faster than chloroform (49). Dichloromethane has also been widely used to produce vesicles by the thin-layer hydration method (50).
Preparation
Vesicle formation
The preparation method greatly influences the size distribution of the vesicular dispersions. Vesicles can be formed by diluting the lamellar bilayer or in the presence of external energy. The frictional force is an external energy that is very influential in forming vesicles (51).
Oleic acid only forms vesicles when the pH equals the pKa of the acid (8.5). Around 50% of the carboxylic acid undergoes ionization at this pH level, transforming into an amphiphile that tends to create vesicles or aggregates (21). Temperature sensitivity is likewise quite high in fatty acid vesicles. Increased thermal agitation caused by high temperatures damages the integrity of fatty acid vesicles (23).
Producing vesicular lipid suspension essentially required vesicle formation and the reduction of particles. Surfactant and lipid mixtures are typically hydrated above the surfactant's gel/liquid transition temperature (Tc) with a drug-containing aqueous solution. The energy input required for vesicle production is either agitation or ultrasonication. Vesicle formation methods already used in novasome production are injection, thin film hydration and vortex.
The injection method has been widely used to make vesicle since it is easier to upscale into a production batch. Slow injection of surfactant/lipid in an organic solution into a hot drug containing aqueous solution is heated to evaporate the above organic solvent above its boiling point (42). Albash et al. have successfully encapsulated fenticonazole by applying the ethanol injection method. First, the drug, span 60, oleic acid, and cholesterol were dissolved in ethanol in a 60ᵒC water bath. The ethanolic solution was injected drop by drop into a fivefold larger volume of distilled water that was magnetically agitated at 60 ᵒC using a magnetic stirrer. In the past, the Brij VR was blended with distilled water. Novasome were generated when sudden turbidity was noted. The mixture was stirred for 30 minutes until all the ethanol evaporated. The result was then exposed to sonication for 5 minutes using a bath-sonicator and a sonicator water bath to reduce the PS. TNs dispersions were then maintained at 4ᵒC (11).
Mosallam et al. successfully utilized ethanol injection to manufacture a novasome loaded with terconazole. The formulation of novasomes involved altering the surfactant type, fatty acid type, surfactant to fatty acid ratio and total lipid concentration. Briefly, ethyl alcohol was employed in a 60°C water bath to dissolve the drug, surfactant, fatty acid, and cholesterol. This was then progressively injected into a five-times bigger volume of phosphate-buffered saline (PBS, pH 7.4) that was magnetically agitated at the same temperature. Seeing sudden turbidity led to the formation of novasome dispersions. The result was continually agitated until all ethanol had evaporated. The resultant novasomes dispersions were then sonicated for particle size reduction (10).
In 1996, Gupta et al. used novasome as an adjuvant for a vaccine. Briefly, two sterile disposable 5 ml syringes were employed for each liposome preparation. One preheated (50°C) syringe contained a lipid combination (dioxyethylene cetyl ether/cholesterol/oleic acid at a molar ratio of 33:11:7) clarified by preheating at 75°C. The second syringe contained 4 ml of 10 mM Dulbecco's phosphate-buffered saline at 65ᵒC, with or without antigen. They connect the syringes with an autoclaved mixing chamber. The lipid phase was injected into the aqueous phase over 1 sec (linear velocity in connector over 10 m/s). The resulting lipid/aqueous combination was returned to the initial syringe within 1 sec. Each cycle was repeated 50 times, with cooling beginning after 15 strokes (formulation temperature between 45 and 50ᵒC). The resulting substance was fluid at room temperature. Before mixing with the lipid, tetanus toxoid (TT) and diphtheria toxoid (DT) was added to the aqueous phase for antigen encapsulation. Antigen was combined with premade novasome in certain tests to achieve the same final concentration as encapsulation trials. Monophosphoryl lipid A (MPL) was dissolved in squalene at 8 mg/ml for encapsulation, and 0.105 ml of MPL in squalene or squalene alone (control) was combined with lipid phase before injection into the aqueous phase (8).
The thin film hydration (TFH) method is based on film formation by evaporation of organic solution containing surfactant/lipid. This film is then hydrated with a drug solution (42). Abd-Elal., et al. have successfully encapsulated zolmitriptan into a novasome vesicle with the TFH method. Cholesterol, drug, free fatty acid, and surfactant were dissolved in chloroform and added to a round-bottomed flask. The organic solvent was progressively evaporated under decreased pressure using a Rotavapor at 60ᵒC until a dry, thin coating formed on the walls of the round-bottom flask. To facilitate the hydration of the thin film, the generated film was hydrated with phosphate buffer saline at pH 7.4 for 1 hour at 60ᵒC with constant stirring using small glass beads. The nanodispersion was refrigerated overnight at 4ᵒC for maturity (9).
Vortex method: In a covered beaker containing ethanol, the weights of the drug, oleic acid, and tween 80 were dissolved in various proportions using the vortex technique. The pH 7 buffer solution was added to the above combination with continuous vortex shaking to produce a cloudy vesicle suspension that was sonicated for 15 minutes to produce tiny vesicles (34).
Size Reduction
The size of vesicles has a significant effect on the in-vivo performance of the active ingredient. The hydration procedure generates microsized vesicles. The nanoscale reduction of vesicle size increases medication release and bioavailability. Combining hydration with optional size-reduction techniques, such as sonication, is recommended (32). Extrusion can be used to reduce the size of liposomes, but it cannot be utilized to create vesicles with ultra-deformable properties; therefore, ultrasonication, whether using an ultrasonic probe or a bath, is an appropriate technique (9–11,34). Probe sonication can produce niosomal vesicle sizes from 100 to 140 nm. Although it is more effective than bath sonication, probe sonication suffers from high energy input to the solution, leading to a sharp local increase in the temperature of the solution and possible shedding of titanium particles into the sonicated dispersion. This necessitates an additional centrifugation step to remove the metallic particles from the vesicle dispersion (42).
To determine the optimal sonication amplitude and duration, optimization is required. If thermolabile is utilized, observing the rise in preparation temperature during sonication is essential. To prevent the preparation from warming, the beaker glass is submerged in an ice bath during the sonication technique (52).
Novasome Characteristic
Elasticity
There are two processes by which vesicles penetrate through the skin layers. The first mechanism involves the vesicles acting as a carrier system by transporting the drug molecule into the skin's stratum corneum. The second mechanism, vesicles, serve as penetration boosters for the intercellular pathway. The lipid layer permits the vesicles to reach the stratum corneum and change the lipids between cells, enhancing fluidity and allowing medications to enter the skin layers (53).
One property distinguishing ultra-deformable vesicles from regular liposomes is their elasticity (with a more rigid membrane). This characteristic permits the vesicles to pass narrow skin-layer gaps smaller than their diameter with minimal risk of rupture (1). Compared to normal liposomes, elastic vesicles have been shown to deposit significantly more active material in the skin (54).
Researchers have discovered elastic niosomes. The development of Tween 60 and Span 60 niosomes containing diclofenac dimethylammonium and 0–25% ethanol. The manufactured niosomes were referred to as elastic niosomes. This is because the produced niosomes registered deformability index values of 13.76, 3.44 times greater than conventionally loaded and unloaded niosomes (55).
Stability
Novasome has demonstrated good stability. The vesicles stored at 4ᵒC and 25ᵒC did not exhibit any clumping or visual alterations. The stability investigation revealed that the vesicles %EE, PS, PDI, and ZP did not change significantly during storage compared to the fresh vesicles (10, 11).
Conclusion
This research highlights the superior properties of novasome technology compared to niosome and ufasome. Novasomes exhibit better vesicle characteristics, higher stability during storage, and better deformability properties. The choice of surfactant, free fatty acid type, and ratio can significantly affect the vesicle characteristics. Novasomes have shown potential as drug carriers and have been applied in various fields, including cosmetics. Ongoing research in this field could lead to the development of smart novasome systems, such as active targeting drug delivery, which could revolutionize drug delivery and improve patient outcomes. The potential applications of novasome technology are vast, and future research will continue to explore new ways to improve their properties and expand their use for various drugs and biomolecule delivery.
Declarations
Acknowledgment
The authors thank the Indonesian Food and Drug Administration for providing material and instruction in writing this review article.
Ethics Statement
Not applicable.
Data Availability
Not applicable.
Funding Information
Not applicable.
Conflict of Interest
The authors declare no conflicting interests.
References
- Ntimenou V, Fahr A, Antimisiaris SG. Elastic vesicles for transdermal drug delivery of hydrophilic drugs: A comparison of important physicochemical characteristics of different vesicle types. J Biomed Nanotechnol. 2012;8(4):613–23.
- Varia U, Joshi D, Jadeja M, Katariya H, Detholia K, Soni V. Development and evaluation of ultradeformable vesicles loaded transdermal film of boswellic acid. Futur J Pharm Sci. 2022;8(1).
- Lin HW, Xie QC, Huang X, Ban JF, Wang B, Wei X, et al. Increased skin permeation efficiency of imperatorin via charged ultradeformable lipid vesicles for transdermal delivery. Int J Nanomedicine. 2018;13:831–42.
- Witika BA, Bassey KE, Demana PH, Siwe-Noundou X, Poka MS. Current Advances in Specialised Niosomal Drug Delivery: Manufacture, Characterization and Drug Delivery Applications. Int J Mol Sci. 2022;23(17).
- Singh A, Malviya R, Sharma PK. Novasome-A Breakthrough in Pharmaceutical Technology a Review Article. Adv Biol Res (Rennes). 2011;5(4):184–9.
- Chambers MA, Wright DC, Brisker J, Williams A, Hatch G, Gavier-Widén D, et al. A single dose of killed Mycobacterium bovis BCG in a novel class of adjuvant (NovasomeTM) protects guinea pigs from lethal tuberculosis. Vaccine. 2004;22(8):1063–71.
- Kaur M, Upadhyay P. A Review on Novasome Technology. 2020;(4).
- Gupta RK, Varanelli CL, Griffin P, Wallah DFH, Siber GR. Adjuvant properties of non-phospholipid liposomes (Novasomes®) in experimental animals for human vaccine antigens (Vaccine (1996) 14/3 (219-225)). Vaccine. 1996;14(8):219–25.
- Abd-Elal RMA, Shamma RN, Rashed HM, Bendas ER. Trans-nasal zolmitriptan novasomes: in-vitro preparation, optimization and in-vivo evaluation of brain targeting efficiency. Drug Deliv. 2016;23(9):3374–86.
- Mosallam S, Ragaie MH, Moftah NH, Elshafeey AH, Abdelbary AA. Use of novasomes as a vesicular carrier for improving the topical delivery of terconazole: In vitro characterization, in vivo assessment and exploratory clinical experimentation. Int J Nanomedicine. 2021;16:119–32.
- Albash R, Ragaie MH, Hassab MA El, El-Haggar R, Eldehna WM, Al-Rashood ST, et al. Fenticonazole nitrate loaded trans-novasomes for effective management of tinea corporis: design characterization, in silico study, and exploratory clinical appraisal. Drug Deliv. 2022 Dec;29(1):1100–11.
- Hasan AA. Design and in vitro characterization of small unilamellar niosomes as ophthalmic carrier of dorzolamide hydrochloride. Pharm Dev Technol. 2014;19(6):748–54.
- Akbari V, Abedi D, Pardakhty A, Sadeghi-Aliabadi H. Ciprofloxacin nano-niosomes for targeting intracellular infections: An in vitro evaluation. J Nanoparticle Res. 2013;15(4).
- Damera DP, Venuganti VV, Pilani S. Deciphering the Role of Bilayer of a Niosome towards Controlling the Entrapment and Release of Dyes. 2018;(April).
- Hunter CA, Dolan TF, Coombs GH, Baillie AJ. Vesicular Systems (Niosomes and Liposomes) for Delivery of Sodium Stibogluconate in Experimental Murine Visceral Leishmaniasis. J Pharm Pharmacol. 2011 Apr;40(3):161–5.
- Yoshioka T, Sternberg B, Florence AT. Preparation and properties of vesicles (niosomes) of sorbitan monoesters (Span 20, 40, 60 and 80) and a sorbitan triester (Span 85). Int J Pharm. 1994 Apr;105(1):1–6.
- Taymouri S, Varshosaz J. Effect of different types of surfactants on the physical properties and stability of carvedilol nano-niosomes. Adv Biomed Res. 2016;5(1):48.
- Gregoriadis G. Engineering liposomes for drug delivery: progress and problems. Trends Biotechnol. 1995;13(12):527–37.
- Kumar L, Verma S, Kumar S, Prasad DN, Jain AK. Fatty acid vesicles acting as expanding horizon for transdermal delivery. Artif Cells, Nanomedicine Biotechnol. 2017;45(2):251–60.
- Hmingthansanga V, Singh N, Banerjee S, Manickam S, Velayutham R, Natesan S. Improved Topical Drug Delivery: Role of Permeation Enhancers and Advanced Approaches. Pharmaceutics. 2022;14(12):1–31.
- Zakir F, Vaidya B, Goyal AK, Malik B, Vyas SP. Development and characterization of oleic acid vesicles for the topical delivery of fluconazole. Drug Deliv. 2010;17(4):238–48.
- Patel DM, Jani RH, Patel CN. Ufasomes: A vesicular drug delivery. Syst Rev Pharm. 2011;2(2):72–8.
- Martin N, Douliez J. Fatty Acid Vesicles and Coacervates as Model Prebiotic Protocells. ChemSystemsChem. 2021;3(6).
- Sinjitha K, Ratnamaala K V. Ufasomes: A Potential Vesicular Drug Delivery System. 2021;8(3):1100–5.
- Rendón A, Carton DG, Sot J, García-Pacios M, Montes R, Valle M, et al. Model systems of precursor cellular membranes: Long-chain alcohols stabilize spontaneously formed oleic acid vesicles. Biophys J. 2012;102(2):278–86.
- Arundhasree, Rajalakshmi R, Aiswarya R, Kumar AR, Kumar SS, Nair SC. Ufasomes: Unsaturated fatty acid based vesicular drug delivery system. Int J Appl Pharm. 2021;13(2):76–83.
- Safer JD, Crawford TM, Holick MF. Topical thyroid hormone accelerates wound healing in mice. Endocrinology. 2005;146(10):4425–30.
- Pushko P, Tumpey TM, Van Hoeven N, Belser JA, Robinson R, Nathan M, et al. Evaluation of influenza virus-like particles and Novasome adjuvant as candidate vaccine for avian influenza. Vaccine. 2007;25(21):4283–90.
- Devi KG, Lakshmi PK. Brain Targeting of Water Soluble Drug Through Nasal Route Using Fatty Acid Vesicles. Int J Pharm Sci Res. 2021;12(2):1177–83.
- Mittal R, Sharma A, Arora S. Ufasomes Mediated Cutaneous Delivery of Dexamethasone: Formulation and Evaluation of Anti-Inflammatory Activity by Carrageenin-Induced Rat Paw Edema Model. J Pharm. 2013;2013:1–12.
- Walde P, Namani T, Morigaki K, Hauser H. Formation and Properties of Fatty Acid Vesicles (Liposomes). Liposome Technol Vol I. 2006;I:1–19.
- Owodeha-Ashaka K, Ilomuanya MO, Iyire A. Evaluation of sonication on stability-indicating properties of optimized pilocarpine hydrochloride-loaded niosomes in ocular drug delivery. Prog Biomater. 2021;10(3):207–20.
- Mustafa AZ. Development of Niosome Containing Roasted Coffee Residue Extract for Antiaging Preparation. 2015;(December 2015).
- N K, R G. Optimization and Evaluation of Oleic Acid Based Unsaturated Fatty Acid Liposomes Gel. J Bioequiv Availab. 2017;09(03):424–9.
- Karal MAS, Mokta NA, Levadny V, Belaya M, Ahmed M, Ahamed MK, et al. Effects of cholesterol on the size distribution and bending modulus of lipid vesicles. PLoS One. 2022;17(1 January):1–24.
- Kumar GP, Rajeshwarrao P. Nonionic surfactant vesicular systems for effective drug delivery—an overview. Acta Pharm Sin B. 2011;1(4):208–19.
- De Mel JU, Gupta S, Willner L, Allgaier J, Stingaciu LR, Bleuel M, et al. Manipulating Phospholipid Vesicles at the Nanoscale: A Transformation from Unilamellar to Multilamellar by an n-Alkyl-poly(ethylene oxide). Langmuir. 2021;37(7):2362–75.
- Lingan MA, Sathali AA asan, Kumar MRV, Gokila A. Formulation and evaluation of topical drug delivery system containing clobetasol propionate niosomes. Sci Rev Chem Commun. 2011;1(1):7–12.
- Yamashita Y, Sakamoto K. Hydrophilic-Lipophilic Balance (HLB): Classical Indexation and Novel Indexation of Surfactant. Encycl Biocolloid Biointerface Sci 2V Set. 2016;1:570–4.
- Aziz DE, Abdelbary AA, Elassasy AI. Fabrication of novel elastosomes for boosting the transdermal delivery of diacerein: Statistical optimization, ex-vivo permeation, in-vivo skin deposition and pharmacokinetic assessment compared to oral formulation. Drug Deliv. 2018;25(1):815–26.
- Devaraj GN, Parakh SR, Devraj R, Apte SS, Rao BR, Rambhau D. Release studies on niosomes containing fatty alcohols as bilayer stabilizers instead of cholesterol. J Colloid Interface Sci. 2002;251(2):360–5.
- Abdelkader H, Alani AWG, Alany RG. Recent advances in non-ionic surfactant vesicles (niosomes): Self-assembly, fabrication, characterization, drug delivery applications and limitations. Drug Deliv. 2014;21(2):87–100.
- Al-Mahallawi AM, Abdelbary AA, Aburahma MH. Investigating the potential of employing bilosomes as a novel vesicular carrier for transdermal delivery of tenoxicam. Int J Pharm. 2015;485(1–2):329–40.
- Manconi M, Caddeo C, Sinico C, Valenti D, Mostallino MC, Biggio G, et al. Ex vivo skin delivery of diclofenac by transcutol containing liposomes and suggested mechanism of vesicle-skin interaction. Eur J Pharm Biopharm. 2011;78(1):27–35.
- Zaki RM, Ali AA, El Menshawe SF, Bary AA. Formulation and in vitro evalution of diacerein loaded niosomes. Int J Pharm Pharm Sci. 2014;6(SUPPL. 2):515–21.
- Sarheed O, Dibi M, Ramesh KVRNS. Studies on the effect of oil and surfactant on the formation of alginate-based O/W lidocaine nanocarriers using nanoemulsion template. Pharmaceutics. 2020;12(12):1–21.
- Kumar P, Singh S, Handa V, Kathuria H. Oleic Acid Nanovesicles of Minoxidil for Enhanced Follicular Delivery. Medicines. 2018;5(3):103.
- Basha M, Abd El-Alim SH, Shamma RN, Awad GEA. Design and optimization of surfactant-based nanovesicles for ocular delivery of Clotrimazole. J Liposome Res. 2013;23(3):203–10.
- Ding X, Han N, Wang J, Sun Y, Ruan G. Effects of organic solvents on the structures of micellar nanocrystals. RSC Adv. 2017;7(26):16131–8.
- Lombardo D, Kiselev MA. Methods of Liposomes Preparation: Formation and Control Factors of Versatile Nanocarriers for Biomedical and Nanomedicine Application. Pharmaceutics. 2022;14(3).
- Naturwissenschaften D Der. Composites of Lyotropic Lamellar Systems and. 2007.
- Nowroozi F, Almasi A, Javidi J, Haeri A, Dadashzadeh S. Effect of surfactant type, cholesterol content and various downsizing methods on the particle size of niosomes. Iran J Pharm Res. 2018;17(Special Issue 2):1–11.
- Marwah MK. Development Of A Novel Deformable Liposomal Formulation For The Dermal Drug Delivery Of Anticancer Agents In The Treatment Of Nonmelanoma Skin Cancers. Aston University. Aston University; 2017.
- Badran M, Shalaby K, Al-Omrani A. Influence of the flexible liposomes on the skin deposition of a hydrophilic model drug, carboxyfluorescein: Dependency on their composition. Sci World J. 2012;2012:1–9.
- Manosroi A, Jantrawut P, Manosroi J. Anti-inflammatory activity of gel containing novel elastic niosomes entrapped with diclofenac diethylammonium. 2008;360:156–63.

 ETFLIN
Notification
ETFLIN
Notification