Pharmacoeconomic Analysis of Drugs Used in Chronic Outpatients at Berkah Pandeglang Regional Hospital
by Yusransyah Yusransyah ★ , Ihda Nurhikmah, Zahra Citra Maharani, Sofi Nurmay Stiani , Afifah Nur Shobah, Baha Udin
Academic editor: Mohd Shahezwan Abd Wahab
Sciences of Pharmacy 4(3): 171-179 (2025); https://doi.org/10.58920/sciphar0403343
This article is licensed under the Creative Commons Attribution (CC BY) 4.0 International License.
05 May 2025
12 Jul 2025
15 Jul 2025
25 Jul 2025
Abstract: Hypertension and type 2 diabetes mellitus (T2DM) are chronic conditions requiring long-term pharmacotherapy, placing significant financial pressure on patients and healthcare systems. Drug selection should prioritize both clinical efficacy and cost-efficiency, particularly in resource-limited settings. This study conducted a pharmacoeconomic evaluation of commonly used therapies at RSUD Berkah Pandeglang using a retrospective, non-experimental design. Data were collected from 2023 outpatient records and analyzed from the hospital’s perspective. Cost-effectiveness was assessed using the Average Cost-Effectiveness Ratio (ACER). For hypertension, amlodipine (n=20) had a lower ACER (Rp 283,913) than candesartan (n=15; Rp 883,000), indicating higher cost-effectiveness. In T2DM patients, metformin (n=25) was more cost-effective (ACER: Rp 317,746.75) than glimepiride (n=25; ACER: Rp 607,148.84). These findings support prioritizing amlodipine and metformin as first-line treatments in similar public healthcare settings to improve therapeutic outcomes while managing costs.
Keywords: Pharmacoeconomic analysisCost-effectiveness of hypertension drugsCost-effectiveness of diabetes medicationAmlodipine vs candesartanMetformin vs glimepirideCost-effective treatment for hypertensionCost-effective therapy for type 2 diabetesACER pharmacoeconomics
Introduction
Chronic non-communicable diseases (NCDs) such as hypertension and type 2 diabetes mellitus are rising rapidly in Indonesia and globally, becoming a major public health and economic burden. According to WHO, NCDs accounted for 74% of all deaths in 2022, with cardiovascular disease and diabetes as leading contributors (1). In Indonesia, hypertension affects 30.8% and diabetes 11.7% of adults, with related healthcare costs exceeding IDR 120 trillion (~USD 8 billion) annually (2, 3). These diseases require lifelong pharmacological treatment, making drug affordability and efficiency a national concern, especially for patients under the BPJS Kesehatan insurance scheme (4).
The standard pharmacotherapy for hypertension includes drugs such as amlodipine and candesartan, while metformin and glimepiride are widely prescribed for diabetes (5). Despite their clinical benefits, these drugs vary significantly in cost and accessibility. More expensive options, such as candesartan or glimepiride, may be necessary in complex cases but can strain public healthcare budgets. In many Indonesian district hospitals, where formularies and funding are limited, the absence of local pharmacoeconomic evaluations forces prescribing decisions to rely more on availability than cost-effectiveness (6-8). Existing national data do not address how these therapies compare in terms of clinical benefit per cost unit, creating a gap in evidence-based prescribing (9, 10).
This study employs pharmacoeconomic analysis, specifically Cost-Effectiveness Analysis (CEA), to compare commonly used monotherapies for hypertension (amlodipine vs. candesartan) and type 2 diabetes (metformin vs. glimepiride) at Berkah Pandeglang Regional Hospital. This district referral facility implements long-term chronic care through Prolanis. By using retrospective real-world data from 2023, the study aims to identify the most cost-effective therapies within this local setting. The findings will help optimize formulary use, inform regional policy, and support rational drug selection in similar resource-constrained environments. This is the first known pharmacoeconomic comparison of these agents at this hospital, offering practical insight into maximizing health outcomes per cost spent.
Methodology
Types of Research
This study employed a retrospective cross-sectional design, a type of observational study that analyzes past patient data at a single point in time to compare the costs and outcomes of different treatment regimens. The research design employed is observational. Data were retrospectively gathered from the medical records of patients with a primary diagnosis of type 2 diabetes mellitus or hypertension without comorbidities, who were included between January and December 2023. The retrospective cross-sectional method was chosen because it allows for efficient and practical comparison of pharmacoeconomic outcomes using existing real-world data without the need for long-term follow-up, making it suitable for hospital-based cost-effectiveness evaluations (11).
This study uses the Cost-Effectiveness Analysis (CEA) approach as the main method in pharmacoeconomic evaluation. CEA is used to compare two different treatment alternatives based on the total costs incurred and the clinical effectiveness obtained, to determine the therapy that provides the best clinical results at the most efficient cost. The pharmacoeconomic analysis in this study was conducted from the payer's perspective. The cost components calculated include direct medical costs, such as drug costs and visit costs, as stated in the medical record data and hospital information system.
Population and Research Sample
The sample in this study was drawn from outpatient medical records of patients diagnosed with type 2 diabetes mellitus or hypertension at Berkah Pandeglang Regional Hospital. The inclusion criteria were defined as patients aged 19 to 70 years, focusing on the adult population with relatively stable treatment patterns and minimizing variability caused by pediatric or geriatric pharmacokinetic differences. Patients were required to be on monotherapy with Amlodipine or Candesartan (for hypertension), or Metformin or Glimepiride (for diabetes), to ensure comparability between drug regimens. Only patients without any documented comorbidities or complications were included, as the presence of such conditions could significantly influence both clinical effectiveness and healthcare costs. Furthermore, the inclusion was limited to those whose medical records were complete for the entire 3-month observational period and who were registered under the BPJS Kesehatan national health insurance scheme, as the study adopted a payer perspective.
Exclusion criteria included patients with complications (such as diabetic nephropathy, cardiovascular disease) or comorbidities (such as asthma or chronic kidney disease), which could confound both treatment selection and outcomes. Patients receiving insulin therapy or combination regimens were excluded to ensure cost-effectiveness comparisons were restricted to standard first-line monotherapy. In addition, patients whose follow-up data (e.g., fasting blood glucose or blood pressure readings) were incomplete, or who transferred to other facilities or died during the observation period, were excluded due to a lack of measurable treatment outcomes. These criteria were applied to ensure internal validity and eliminate clinical and economic biases in evaluating the cost-effectiveness of the selected drug therapies.
The sample size was determined using a total sampling technique from all eligible patients who met the inclusion criteria during the study period (January–December 2023). No power calculation was required due to the study's retrospective nature and the use of complete enumeration of available records. From the hospital database, a total of 176 patient records (92 with hypertension and 84 with type 2 diabetes mellitus) were included in the final analysis. Sampling was non-random but purposive, based on defined clinical and data completeness criteria to ensure reliable comparison across pharmacoeconomic indicators. This approach is common in retrospective cost-effectiveness studies that use real-world data, where full population data are available.
Clinical Outcomes
Clinical effectiveness in this study was assessed based on clinical parameters commonly used to evaluate therapy for hypertension and type 2 diabetes mellitus. Effectiveness parameters in hypertension were measured based on a decrease in systolic blood pressure (SBP) and diastolic blood pressure (DBP) after at least 4 weeks of routine drug use. Treatment was declared effective if the patient achieved a blood pressure <140/90 mmHg according to the therapy target based on the European Society of Hypertension 2023 guidelines (9). Conversely, therapy was considered ineffective if blood pressure remained at≥140/90 mmHg, even though treatment had been administered according to the recommended dose. Meanwhile, patients with type 2 diabetes mellitus were measured based on a decrease in fasting blood glucose (FBS) levels after at least 8 weeks of treatment. Therapy was considered effective if FBS levels were <130 mg/dL, according to the standards set by the American Diabetes Association (ADA) 2024 (10). Conversely, therapy was considered ineffective if FBS levels remained ≥130 mg/dL after routine therapy.
Data Retrieval
The data in this study were obtained from patient medical records and direct medical cost data gathered from the administration and finance department of Berkah Pandeglang Regional Hospital in 2023. The cost data included only direct medical costs, which consisted of visiting fees and drug costs. Drug costs were extracted from the hospital pharmacy records, while visiting costs were based on the hospital’s official tariffs for BPJS Kesehatan participants.
Access to patient medical records and hospital billing data was officially granted through institutional research permits issued by the Health Research Ethics Committee of Prof. Dr. Hamka Muhammadiyah University with approval letter numbers 03/24.02/03147 and 03/24.02/03150. A trained team of two clinical pharmacists and one health economist conducted the data collection under the supervision of a senior researcher. Data were extracted manually using a standardized data abstraction form that had been pilot-tested before use. To ensure data integrity, double data entry and cross-verification procedures were implemented, with discrepancies resolved through consensus by the research team. Patient identifiers were anonymized and coded before analysis to ensure confidentiality. The data collection process followed ethical and procedural guidelines consistent with national standards for secondary data research in healthcare (12).
Data Analysis
Analysis of data in this study was carried out using the ACER calculation. Patient medical record data were then run through Microsoft Excel as number processing software. After the data were gathered, they were analyzed and processed using the ACER formula to determine the cost-effectiveness of various therapies implemented (13).
The Average Cost-Effectiveness Ratio (ACER) was calculated by dividing the total treatment cost by the number of patients achieving the defined clinical outcome, representing the cost per successful outcome. For hypertension, effectiveness was defined as achieving blood pressure <140/90 mmHg. For diabetes mellitus, effectiveness was defined as achieving fasting blood glucose <130 mg/dL. These thresholds were based on the 2023 European Society of Hypertension and 2024 ADA guidelines, respectively.
No | Characteristics | Category | Frequency (n) | Percentage (%) |
1 | Sex | Male | 10 | 29% |
Female | 25 | 71% | ||
2 | Age Group | 20–30 Years | 7 | 20% |
31–40 Years | 3 | 8% | ||
41–50 Years | 6 | 17% | ||
51–60 Years | 9 | 26% | ||
61–70 Years | 10 | 29% | ||
3 | Frequency of Visits | 3 Visits | 18 | 51% |
>3 Visits | 17 | 49% |
No | Characteristic | Category | Frequency (n) | Percentage (%) |
1 | Sex | Male | 15 | 30% |
Female | 35 | 70% | ||
2 | Age Group | Adults (19–59 years) | 27 | 54% |
Elderly (60–70 years) | 23 | 46% | ||
3 | Frequency of Visits | 3 Visits | 18 | 36% |
>3 Visits | 32 | 64% |
Variables measured in this analysis included total treatment cost per patient (IDR), blood pressure or fasting blood glucose outcome (effective or ineffective), age, sex, and drug regimen used. Descriptive statistics were performed to describe patient characteristics and costs. However, Microsoft Excel was used for initial data processing, ACER calculation, and data validation.
Result and Discussion
Characteristics of Hypertension Patients
Data gathering was conducted at the Medical Records Installation using a purposive sampling method. A total of 35 patients were selected as samples and grouped into two: the amlodipine group (20 patients) and the candesartan group (15 patients). Quantitative data, including patient characteristics, were computed using Microsoft Excel and expressed in percentage terms for easy interpretation and comparison across groups.
Table 1 shows that patients diagnosed with hypertension at Pandeglang Berkah Regional Hospital in 2023 were female-predominant among the population. The results confirm previous studies claiming that women, especially postmenopausal women (over 45 years of age), are more susceptible to high blood pressure. Non-menopausal women are generally protected by the hormone estrogen, which has a function to increase levels of high-density lipoprotein (HDL), a factor that may be protective against hypertension (14).
As shown in Table 1, the subjects of this study were categorized into five age groups, and the 61-70 years age group (29%) suffered the most from hypertension. The incidence of hypertension is indeed age-related, where the older one gets, the more likely one is to suffer from hypertension. Therefore, the older population is at greater risk of suffering from hypertension, with a prevalence rate of up to 40%, and a higher mortality rate among individuals above age 60. The larger lumen of blood vessels decreases as age progresses, and the walls of blood vessels become stiffer (15). However, adolescents are also possibly plagued with hypertension due to unwholesome lifestyles, such as inappropriate food consumption, excessive fat, overweight, stress, and lack of exercise. In addition, genetic factors can also significantly contribute to causing hypertension at a young age (16).
Regarding the length of outpatient care for hypertension patients at Pandeglang Berkah Regional Hospital, Berkah Pandeglang, in 2023, the duration of the visit varies. More severely ill patients need more frequent visits and longer treatment compared to patients who are improving. The number of visits affects the effectiveness of the use of the administered drugs.
Characteristics of Type 2 DM Patients
Data collection was conducted in the Medical Records Installation, Outpatient Installation, and Laboratory. The data collection approach used purposive sampling, whereby a sample of 100 patients was selected. From this number, 50 patients were enrolled who met the inclusion criteria, which included two therapy groups: the metformin therapy group with 25 patients and the glimepiride therapy group with 25 patients.
Based on Table 2, the majority of patients with type 2 diabetes mellitus at Pandeglang Berkah Regional Hospital, Pandeglang, are females, at a rate of 70%. This is due to the presence of some of the higher risk factors among women for type 2 diabetes, including PCOS (Polycystic Ovary Syndrome), hormonal imbalance, menopause, obesity, fat distribution, and physical inactivity, which can cause insulin resistance. Though these raise the risk, they are not causes of type 2 diabetes. Women with one or more of these risk factors will not necessarily develop type 2 diabetes, but their risk is raised. Prevention through healthy living, i.e., a good diet and regular exercise, is therefore the best way to reduce the risk of developing type 2 diabetes (14).
As per Table 2, the subjects of this research were grouped into two age groups, namely adults and the elderly. The predominant age group affected by type 2 diabetes mellitus is the adult age group (19-59 years), with 27 patients (54%). This is perhaps because the function of body cells, including those that secrete insulin, weakens, and also because body metabolism tends to slow down with increasing age. These results suggest that type 2 diabetes can occur at a vulnerable age in adulthood, as it is associated with a decrease in pancreatic cell function and insulin secretion, which can lead to improved insulin resistance among adults (14).
These results are in line with research by Dedy (2015), which describes diabetes as becoming more common in late life. It is caused by the decline in human physiological status, specifically through the aging process, coupled with changes in body composition and neurohormonal changes. Particularly, the decline of Insulin-like Growth Factor-1 (IGF-1) and dehydroepiandrosterone (DHEA) in plasma can worsen the condition. A decrease in IGF-1 leads to a reduction in the body's glucose uptake due to decreased receptor sensitivity and impaired insulin action. Conversely, a decrease in the level of DHEAS is associated with high levels of body fat and low physical activity, which also worsen insulin resistance. It is also worsened by the patient's lifestyle change, which is primarily unhealthy (15).
Outpatient care for patients with type 2 diabetes mellitus at Berkah Pandeglang Regional Hospital in 2023 has a varying frequency of visits, which can be based on the patient's condition. The frequency of visits referred to here is the number of monthly visits by type 2 DM patients undergoing outpatient care. These patient visits correspond to the level of success of outpatients' treatment of diabetes from January to December 2023, as evaluated by fasting blood sugar test results. Patients will be required to visit more frequently and undergo longer treatment in the outpatient setting if their blood glucose levels are not significantly decreased. Based on Table 1, the majority of patients have a total of more than three visits.
The three main determinants, as stated by Saibi (2020), that influence the effectiveness of treatment being low include lifestyle, level of compliance, and drug intake. The patient in this case is subjected to ineffective treatment on a monthly basis, as evidenced by the irregularity of patient visits. The ineffectiveness of treatment may reduce the therapeutic value of the administered therapy, making it suboptimal and poorly controlled (16).
Cost-Effectiveness Analysis of Hypertension Patients
The costs accounted for in this research are direct medical costs, i.e., all expenses incurred by patients regarding medical care for hypertension treatment. In this study, the direct medical cost data obtained consisted of drug costs and visit costs.
Cost analysis is an important part of health planning, as it determines the cost of a program or a unit of a health service and helps reach the total budget needed. In this study, the visit costs were established by multiplying the visit cost per patient by the number of patients visited. In contrast, total drug costs were calculated based on the amount of drugs administered to each patient during each visit. From Table 3, the average total cost in the candesartan group was higher than in the amlodipine group. Low-cost, effective treatment is the optimal therapeutic management, especially in hypertensive patients. Therefore, a cost-effectiveness analysis of oral antihypertensive drug use in hypertensive patients is necessary to provide optimal treatment options, considering effective treatment costs (16). Cost comparison between treatment groups indicates that candesartan incurs a significantly higher total direct cost than amlodipine. This supports existing evidence that angiotensin receptor blockers tend to be more expensive than calcium channel blockers, particularly in generic-restricted formularies (20). The implication is that while both agents are clinically viable, amlodipine offers a more affordable first-line choice in resource-limited public healthcare settings.
Cost estimation is an important component of planning health to calculate the cost of a program or unit of a health service, and to determine the overall budget requirement. In this study, visit cost outcomes were computed by multiplying the visit cost per patient by the number of patients visited, whereas overall drug cost was calculated using the number of drugs administered per visit to each patient. According to Table 3, the mean total cost in the candesartan group was higher compared to the amlodipine group. Low-cost, effective therapy is the optimal therapy management, especially in hypertensive individuals. Therefore, cost-effectiveness analysis of oral antihypertensive drug use in hypertensive patients is most needed to provide the optimal treatment options in the form of effective treatment costs.
The assessment of the effectiveness of hypertension therapy is conducted by observing the decrease in systolic blood pressure (SBP) and diastolic blood pressure (DBP) after the patient has taken the medication regularly for at least four weeks. Therapy is considered effective if the patient's blood pressure decreases to below 140/90 mmHg, as per the European Society of Hypertension guidelines in 2023 (9). Conversely, if blood pressure remains ≥140/90 mmHg even after treatment has been administered according to the recommended dose, the therapy is considered unsuccessful.
To operationalize this definition, each patient's blood pressure before initiating treatment (baseline) was compared to their most recent reading after at least four weeks of continuous therapy. Only patients with documented baseline and follow-up values were included. Patients were classified as “effective” if their follow-up SBP was <140 mmHg and DBP <90 mmHg, regardless of the magnitude of change from baseline (see Table 4). This approach aligns with the clinical target thresholds recommended by ESH 2023 for outpatient hypertension management (21).
Cost Component | Amlodipine | Candesartan |
Visiting Fees | IDR 19,404,000 | IDR 23,958,000 |
Drug Costs | IDR 469,910 | IDR 766,320 |
Total Direct Medical Cost | IDR 19,873,910 | IDR 24,724,320 |
Average Cost per Patient | IDR 993,696 | IDR 1,648,288 |
Drug Group | Total Patients | Effective (n) | Effective (%) | Ineffective (n) | Ineffective (%) |
Amlodipine | 20 | 14 | 70% | 6 | 30% |
Candesartan | 15 | 4 | 28% | 11 | 72% |
Therapy Group | Total cost | Effectiveness (%) | ACER (Total Cost/Effectiveness) |
Amlodipine | IDR 19,873,910- | 70 | IDR 283,913- |
Candesartan | IDR 24,720,000- | 28 | IDR 883,000- |
The results of this study align with the research of Akbar et al. (2024), which states that calcium channel blocker-type antihypertensive drugs are effective in lowering blood pressure in patients with volume overload-induced hypertensive disease, such as dialytic hypertensive patients. CCB can therefore be used as a first-line treatment for hypertension. This is because calcium channel blocker drugs, such as amlodipine, not only target blood vessel muscle, but also heart muscle. Amlodipine can reduce cardiac output, hence reducing blood volume and blood pressure. However, both amlodipine and candesartan function by inhibiting calcium flow and angiotensin receptors, thereby causing blood vessels to relax and dilate, and effectively lowering blood pressure (16).
According to Table 5, the lowest-priced treatment for hypertension patients at the Berkah Pandeglang Hospital Outpatient Pharmacy Installation in 2023 was the amlodipine group, with an ACER value of IDR 283,913, and the candesartan group, which equaled IDR 883,000. The results of this study concur with the research of Perawati et al. (2021), conducted in a hospital in Jambi, which found that the use of amlodipine was more economical than the use of candesartan, based on the treatment duration outcome (22).
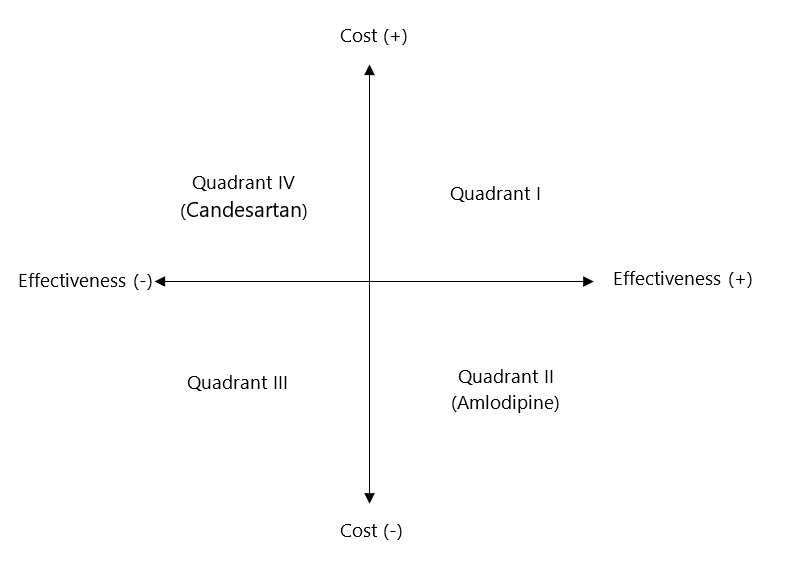
The ACER value indicates the cost required for every 1% improvement in treatment effectiveness. A lower ACER combined with higher therapeutic effectiveness reflects a more economical use of the drug. Based on this study, amlodipine was the most cost-effective option for treating hypertension in outpatients at Berkah Pandeglang Regional Hospital (22). In the cost-effectiveness quadrant analysis, quadrant I represents high effectiveness with high cost, quadrant II indicates high effectiveness with the lowest cost, quadrant III shows low effectiveness with low cost, and quadrant IV reflects low effectiveness with the highest cost (23).
As can be seen from Figure 1, amlodipine drug therapy has a low total cost and high effectiveness, and therefore it lies in quadrant II. But candesartan drug therapy has a high total cost and low effectiveness, and thus it lies in quadrant IV. Based on the outcome of these quadrants, no further consideration with ICER calculations is required. This aligns with the belief of Andayani (2013), who clarified that ICER can be calculated when the drug therapy is more expensive but more effective, or when the therapy cost is less expensive but less effective. ICER is used to characterize the amount of added costs per unit of health improvement (20).
Cost-Effectiveness Analysis of Type 2 Diabetes Mellitus Patients
The expenses in this research are defined as direct medical expenses, meaning all expenses incurred by patients concerning medical services for the treatment of diabetes mellitus (DM). These expenses include consultation fees, medication costs, and other expenses directly related to the treatment and management of DM patients.
Table 6 describes the data on the medical costs used in this research. The direct medical costs used in this research were estimated as visit costs, drug costs, total costs, and average costs. This cost analysis is conducted from the payer's perspective, where BPJS insurance reimburses medical costs. Visit prices are set by the price of a single visit in package form, which is IDR 198,000, and then multiplied by patient visit frequency. Prices of drugs are set by the price of a single drug visit multiplied by the frequency of visits. Prices for a single visit of metformin are IDR 8,106, and for glimepiride, it is IDR 21,357. The total cost is determined by adding the total cost of the visit and the total cost of the medication. According to the findings of this study, the glimepiride group had a higher average total cost compared to the metformin group.
The economic evaluation reveals that metformin is a more cost-effective antidiabetic agent compared to glimepiride. This finding is consistent with global pharmacoeconomic data, which favor metformin due to its low cost and reliable glycemic control, making it a cornerstone of type 2 diabetes treatment, especially in low- to middle-income countries (21). Its lower acquisition cost, minimal risk of hypoglycemia, and wide availability enhance its value in public insurance systems, such as BPJS Kesehatan.
No | Cost Analysis | Metformin | Glimepiride |
1 | Visiting Fees | IDR 21,978,000 | IDR 30,690,000 |
2 | Drug Costs | IDR 899,766 | IDR 3,310,335 |
3 | Total cost | IDR 22,877,766 | IDR 34,000,335 |
4 | Average | IDR 915,110 | IDR 1,360,013 |
Effective | % | Ineffective | % | |
Metformin | 18 | 7 | 28% | |
Glimepiride | 14 | 11 | 44% |
Drug Therapy | Total Cost (IDR) | % Effectiveness | ACER (IDR) |
Metformin | IDR 22,877,766 | 72% | IDR 317,746 |
Glimepiride | IDR 34,000,335 | 56% | IDR 607,148 |
The results of this study are consistent with a research study by Priharsi (2015), which concluded that the average total cost of outpatient type 2 DM treatment for BPJS members at Dr. Moewardi Hospital in 2014 was the highest for sulfonylurea therapy, i.e., IDR 225,008 ± 64,305.93 (18). The other study, conducted by Meliawati (2023), also found that the lowest direct medical cost was associated with the use of metformin drug therapy, at IDR 4,227,493. In contrast, the use of glimepiride therapy had the highest total direct medical cost, amounting to IDR 5,234,019.
Therapeutic efficacy in this research was quantified based on the control of fasting blood glucose (FBS) levels that attained the therapy target. This quantification was achieved by comparing the percentage of FBS levels that successfully attained the therapy target on the third-month test. The therapy target of FBS levels according to ADA 2015 is 80-130 mg/dl. The ratio of FBS levels achieving the target was calculated by dividing the number of controlled FBS data points by the total measurement of FBS levels for each treatment group (26).
The effectiveness of fasting blood glucose (FBS) control was measured by comparing the patient’s baseline FBS values with their FBS result after at least 8 weeks of therapy. The cutoff for therapeutic success was defined as FBS <130 mg/dL, based on ADA 2024 standards. The baseline was recorded from the earliest available FBS before initiation of drug therapy, and follow-up FBS was taken from the third-month laboratory report. Patients were considered “effective” if their follow-up FBS fell below this threshold, regardless of the magnitude of change. This absolute threshold method reflects real-world decision-making standards used in clinical guidelines and insurance reimbursement (27).
Based on Table 7, we can see that the metformin drug group has a higher effectiveness value compared to the glimepiride drug group. This is in line with the study findings of Priharsi (2015), which showed that oral antidiabetics in the Biguanide group (e.g., metformin) have the highest therapeutic effectiveness, with an effectiveness percentage of 58.33%, while the Sulfonylurea group (e.g., glimepiride) had the lowest effectiveness, i.e., 14.81% (18). Rafie's (2023) study also supports these findings, where patients undergoing metformin therapy and achieving the therapy target of 33 out of 38 patients had an effectiveness value of 86.84%. In patients undergoing glimepiride therapy, 20 out of 27 patients achieved the therapy target, with an effectiveness value of 74.07%.
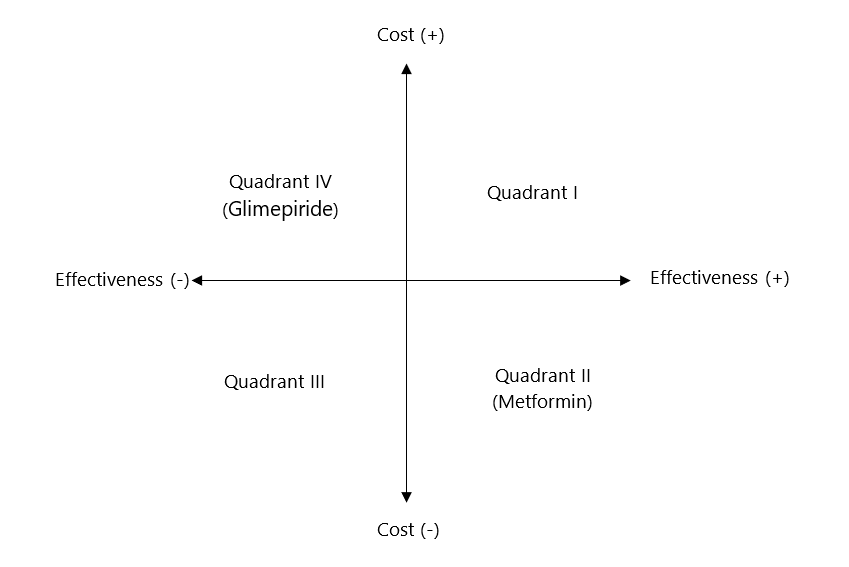
Table 8, in turn, demonstrates that the total cost was lower among the metformin drug treatment group, at IDR 22,877,766.00, and the efficacy level thereof (72%), when compared to that for glimepiride, at IDR 34,000,335.00, but significantly less, at an efficacy rate of 56%. Based on the results of the ACER value calculation, metformin drug therapy was more cost-effective than glimepiride therapy. The ACER value of metformin therapy was IDR 317,746.75, which was cheaper than that of glimepiride therapy, at IDR 607,148.839. Wahyu (2018) in his study elucidated that an array of therapies was declared as the most cost-effective when it possessed a lower ACER value than other arrays of therapy (20). Drug therapy with metformin was found to be more effective and less expensive in this analysis and hence falls under the dominant category and does not require ICER calculations.
The results of this study align with those of Ni Wayan (2023), who reported the highest efficacy in the single biguanide therapy treatment pattern, at 97.30%. The most cost-effective treatment in the study was single biguanide therapy, with an ACER value of IDR 579.23, producing benefits of IDR 261.02. In addition, the results of Meliawati's (2023) study also showed that the maximum ACER value was obtained under glimepiride drug treatment, with a result of IDR 73,718, while the minimum ACER value was shown by metformin drug treatment, which was IDR 49,156 (18).
From Figure 2, metformin drug treatment is characterized as having a low total cost with high effectiveness, and therefore it falls in quadrant II. On theother hand, glimepiride drug treatment has a high total cost with low effectiveness, so it falls in quadrant IV. According to the findings of the quadrants, no further consideration is required using the ICER calculation. This is consistent with Andayani's (2013) perception, who believed that ICER can be calculated when a drug therapy is more expensive but more effective, or when therapy is less expensive but less effective. ICER is used to determine the additional costs per unit of health improvement (20).
Factors Influencing Cost-Effectiveness Outcomes
Based on the ACER values and quadrant analysis, Amlodipine and Metformin were found to be more cost-effective than their comparators, Candesartan and Glimepiride, respectively. These findings suggest their superiority in delivering therapeutic benefit at a lower cost.
The superior cost-effectiveness of amlodipine may be attributed to both its pharmacological profile and market accessibility. Amlodipine, a calcium channel blocker, has a long plasma half-life and can be administered once daily, which may improve patient adherence and stabilize blood pressure over time (28). It is also widely available as a low-cost generic medication, resulting in significantly lower procurement costs in public healthcare settings. Candesartan, although effective, is often more expensive due to limited generic competition and more complex manufacturing processes.
Similarly, Metformin is considered the gold standard for first-line therapy in type 2 diabetes. Its cost advantage is supported by its simple production, long-standing market presence, and broad availability on national formularies. Clinically, metformin improves insulin sensitivity without increasing insulin secretion, resulting in a lower risk of hypoglycemia compared to sulfonylureas, such as glimepiride. This mechanism not only enhances safety but may also contribute to better long-term glycemic control (29). These pharmacologic and economic factors likely explain its superior cost-effectiveness in the present study.
In the management and treatment of type 2 diabetes mellitus, the selection of the right therapeutic regimen not only considers clinical effectiveness but also cost efficiency. Therefore, a comparison between amlodipine and candesartan, as well as between metformin and glimepiride, becomes relevant to be explained pharmacoeconomically.
Based on the literature, amlodipine and candesartan have different efficacy in terms of blood pressure control and target organ protection effects. A study by Mhmndar et al. (2025) demonstrated that candesartan was superior to amlodipine in consistently lowering systolic blood pressure and protecting kidney function, particularly in patients with high cardiovascular risk (30). Although both are first-line therapies according to the ESH 2023 guidelines, the non-identical clinical effectiveness between the two underlies the need for evaluation from a pharmacoeconomic perspective (9).
The comparison of metformin and glimepiride is supported by several studies that demonstrate differences in glycemic control, risk of hypoglycemia, and side effect profiles. According to research by Chandrappa et al. (2024), glimepiride lowers blood glucose levels more quickly but has a higher risk of hypoglycemia compared to metformin. In contrast, metformin has a better safety profile and additional benefits on body weight and insulin resistance (31). The 2024 ADA guidelines also emphasize that the effectiveness of these two drugs is not identical and the choice of therapy needs to be adjusted to the patient's clinical condition (10).
Thus, there is scientific evidence indicating that the two drug pairs have different effectiveness, making a comparative analysis from a pharmacoeconomic perspective relevant, especially in the context of public health services in Indonesia.
Policy Implications and Relevance to National Health Insurance
These findings carry important implications for national health insurance policy, particularly within the BPJS Kesehatan system. The demonstrated cost-effectiveness of amlodipine over candesartan and metformin over glimepiride suggests that these drugs should be prioritized in formulary recommendations, therapeutic guidelines, and procurement strategies. BPJS Kesehatan could use this evidence to advocate for preferential coverage, bulk purchasing agreements, or tiered reimbursement models that favor cost-effective treatments. Such strategies could potentially reduce budgetary pressure while maintaining or even improving treatment outcomes at the population level.
Moreover, the study highlights the potential influence of patient compliance and drug accessibility on therapeutic effectiveness. For instance, higher visit frequencies observed in less effective therapy groups may reflect underlying issues such as poor adherence, suboptimal patient education, or barriers to consistent medication access, factors that are especially relevant in remote or underserved regions. Addressing these elements through patient counseling, simplified dosing regimens, and ensuring drug availability at first-level health facilities can further enhance cost-effectiveness in real-world settings.
Ultimately, integrating pharmacoeconomic analysis into BPJS policy development could support evidence-based decisions and help balance clinical benefits with sustainable financing. This is especially urgent given the increasing burden of chronic diseases, such as hypertension and type 2 diabetes, which are leading cost drivers in the Indonesian healthcare system.
In light of these findings, it is recommended that Berkah Pandeglang Regional Hospital continue to prioritize Amlodipine and Metformin as first-line options in routine outpatient care for hypertension and type 2 diabetes, respectively. However, Candesartan and Glimepiride should remain available in the hospital formulary for specific patient groups who may benefit more from these agents based on clinical indications, such as patients with high cardiovascular risk or those unresponsive to standard therapies. To support this, the hospital is advised to strengthen its clinical assessment and stratification protocols, including regular renal and metabolic monitoring, to ensure the selection of appropriate drugs tailored to individual patient needs. This approach allows the hospital to align clinical decision-making with pharmacoeconomic evidence while maintaining flexibility for case-based treatment.
Conclusion
This study found that amlodipine is more cost-effective than candesartan for treating hypertension (ACER: IDR 283,913 vs. IDR 883,000), and metformin is more cost-effective than glimepiride for treating type 2 diabetes (ACER: IDR 317,746.75 vs. IDR 607,148.84). Their superior cost-effectiveness is attributed to better affordability, clinical efficiency, and wider availability. Amlodipine’s once-daily dosing and long half-life improve adherence, while metformin’s insulin-sensitizing effect and low hypoglycemia risk make it a strong first-line choice. These findings support the prioritization of amlodipine and metformin in outpatient care at public hospitals. However, further research with larger samples, multicenter data, and broader cost assessments is recommended to validate these results and guide national healthcare policy.
Declarations
Ethics Statement
This research has obtained ethical feasibility permit from the Health Research Ethics Committee (Non-Medical) of Prof. Dr. Hamka Muhammadiyah University with letter number 03/24.02/03150 and 03/24.02/03157.
Data Availability
The data used in this study are stored securely by the researchers and cannot be published publicly to maintain the confidentiality of patient information and comply with the principles of research ethics. Access to data can only be given to authorized parties in accordance with ethical approval and related institutional policies.
Funding Information
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of Interest
The authors declare no conflicting interest.
References
- WHO. Noncommunicable-Diseases [Internet]. 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
- Kementerian Kesehatan Republik Indonesia. Prevalence , Impact , and Efforts In Controlling Hypertension & Diabetes in Indonesia. 2023;1–2. Available from: https://www.bps.go.id/id/statistics-table/2/MTQ4MCMy/prevalensi-tekanan-darah-tinggi-menurut-provinsi.html
- International Diabetes Federation. International Diabetes Federation. 2023 [cited 2025 Jul 14]. IDF Diabetes Atlas, 10th edition. Available from: https://diabetesatlas.org/
- BPJS Kesehatan. Laporan Pengelolaan Program dan Keuangan BPJS Kesehatan Tahun 2022 [Internet]. Bpjs Kesehatan. 2023. Available from: https://www.bpjs-kesehatan.go.id/bpjs/arsip/detail/2169
- Baroroh F, Sari A, Masruroh N. Cost effectiveness analysis of candesartan therapy in comparison to Candesartan-Amlodipine therapy on hypertensive outpatients. Open Access Maced J Med Sci. 2019;7(22):3837–40.
- Amalia A, Suardiana IK. The Role of Pharmacoeconomics in Determining Treatment Selection in Indonesia: A Scoping Review. Journal of Pharmaceutical Science and Application. 2025 Jun 27;7(1):40–50.
- Yuniarti E, Prabandari YS, Kristin E, Suryawati S. Rationing for medicines by health care providers in Indonesia National Health Insurance System at hospital setting: a qualitative study. J Pharm Policy Pract. 2019 Dec 7;12(1):7.
- Yuniar Y, Herman MJ. Overcoming Shortage of Pharmacists to Provide Pharmaceutical Services in Public Health Centers in Indonesia. Kesmas: National Public Health Journal. 2013 Jul 1;8(1):3.
- Limato R, Lazarus G, Dernison P, Mudia M, Alamanda M, Nelwan EJ, et al. Optimizing antibiotic use in Indonesia: A systematic review and evidence synthesis to inform opportunities for intervention. The Lancet Regional Health - Southeast Asia. 2022 Jul;2:100013.
- Hidayat B. Evolution of Health Technology Assessment in Indonesia: Supply Landscape, Implementation, and Future Directions. Health Syst Reform. 2023 Dec 31;9(3).
- Lee W, Dayer V, Jiao B, Carlson JJ, Devine B, Veenstra DL. Use of real-world evidence in economic assessments of pharmaceuticals in the United States. J Manag Care Spec Pharm. 2021;27(1):5–14.
- Lestari AY, Misran, Raharjo T, Annas M, Riskanita D, Prabandari AP. Improving Healthcare Patient Data Security: An Integrated Framework Model For Electronic Health Records From A Legal Perspective. Law Reform J Pembaharuan Huk. 2024;20(2):329–52.
- Khoiriyah SD, Lestari K. Kajian Farmakoekonomi yang Mendasari Pemilihan Pengobatan di Indonesia. Farmaka. 2018;16(3).
- Masnah C, Daryono D. Efektivitas Media Edukasi Booklet dalam Meningkatkan Dukungan Keluarga dan Kepatuhan Pengobatan Penderita Hipertensi. J Ilmu Kesehat Masy. 2022 May 13;11:213–22.
- Nababan OA, Oktadiana I, Prasetyawan F, Saristiana Y, Muslikh FA, Mildawati R. Evaluasi Penggunaan Obat Pada Pasien Hipertensi Rawat Jalan Di Puskesmas “X” Kota Solo. J Media Akad. 2024;2(2).
- Akbar DO, Yaumil F, Setiawan AA. Analisis Efektivitas Biaya Pengobatan Hipertensi Pada Pasien Rawat Jalan Di Klinik Nurul Hasanah Tahun 2022. J Insa Farm Indones. 2024;6(3):9–17.
- Marzuk RH, Oetari RA, Hanifah IR. Analisis Efektivitas Biaya Terapi Metformin dan Glimepiride pada Pasien Diabetes Melitus Tipe 2 di RSUD dr. Darsono Pacitan Tahun 2019. J Ilmu Farm dan Farm Klin. 2023;20(1):20.
- Almasdy D, Sari DP, Suhatri S, Darwin D, Kurniasih N. Evaluasi Penggunaan Obat Antidiabetik Pada Pasien Diabetes Melitus Tipe-2 di Suatu Rumah Sakit Pemerintah Kota Padang – Sumatera Barat. J Sains Farm Klin. 2015;2(1):104.
- Anisawati Amanda, Pratama KJ, Artini SK. 2835-Article Text-5079-2-10-20230704. 2023;84–92.
- Hasanah NU, Dewi NMAR, Saputra YD. Cost-effectiveness analysis of amlodipine and candesartan in the inpatient setting at Mataram University Hospital in Indonesia, 2021. Pharm Educ. 2024;24(3):228–33.
- Tandon T, Dubey AK, Saurabh S, Manocha S, Arora E, Hasan N. A pharmacoeconomic analysis to compare cost‑effectiveness of metformin plus teneligliptin with metformin plus glimepiride in patients of type‑2 diabetes mellitus. J Fam Med Prim Care [Internet]. 2017;6(2):169–70. Available from: http://www.jfmpc.com/article.asp?issn=2249-4863;year=2017;volume=6;issue=1;spage=169;epage=170;aulast=Faizi
- Perawati S, Andriani M, Utaka T. Analisis Efektifitas Biaya Penggunaan Obat Hipertensi Amlodipin Dan Candesartan Pada Pasien Bpjs Rawat Inap Di Rumah Sakit Dr. Bratanata Jambi Tahun 2019. Pharma Xplore J Ilm Farm. 2021;6(2):47–54.
- Kolbiyah L. Analisis Efektivitas Biaya Penggunaan Antibiotik pada Pasien Pnemonia Rawat Inap di RSU Karsa Husada Kota Batu tahun 2017-2018. 2019;
- Wuryandari H, Raising R, Widiarini R. ANALISIS EFEKTIVITAS BIAYA TERAPI ANTIDIABETES ORAL KOMBINASI PADA PASIEN DIABETES MELITUS TIPE 2 DI RSUD KOTA MADIUN TAHUN 2020. 2021;1(2).
- Meliawati NW, Lolo widya A, Rundengan G e. Analisis efektivitas biaya penggunaan metformin dan glimepiride pada pasien diabetes melitus tipe 2 rawat inap di RS. robert Wolter monginsidi kota Manado. Pharm Med J. 2023;6(1):68–76.
- Tetuko A, Nugraheni DA. ANALISIS EFEKTIFITAS BIAYA KOMBINASI ANTIDIABETIK ORAL PADA PASIEN RAWAT JALAN DIABETES MELITUS TIPE 2. 2021;5(2):105–16.
- Dhatariya K, Umpierrez GE. Management of Diabetes and Hyperglycemia in Hospitalized Patients [Internet]. South Dartmouth: MDText.com; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279093/
- Chan L, Chen CH, Hwang JJ, Yeh SJ, Shyu KG, Lin RT, et al. Cost-effectiveness of amlodipine compared with valsartan in preventing stroke and myocardial infarction among hypertensive patients in Taiwan. Int J Gen Med. 2016;9:175–82.
- Soiza RL, Donaldson AIC, Myint PK. Vaccine against arteriosclerosis: an update. Ther Adv Vaccines. 2018;9(6):259–61.
- Mhmndar MA, Singh T, Fatima I, Shehryar A, Zaidi MR, Mairaj M, et al. Comparative Efficacy and Safety of Angiotensin-Converting Enzyme Inhibitors, Angiotensin Receptor Blockers, and Calcium Channel Blockers in Hypertensive Patients With Chronic Kidney Disease: A Systematic Review. Cureus. 2025 Feb;17(2):e78845.
- Chandrappa S, Shetty S, Narayana AT, Rajarathna K. A comparative study of efficacy and safety of glimepiride versus gliclazide as an add on to metformin in Type 2 diabetes mellitus at a tertiary care hospital. Natl J Physiol Pharm Pharmacol. 2024;14(09):1824–30.

 ETFLIN
Notification
ETFLIN
Notification








