Prevalence, Causes, and Management Strategies of Fungal Diseases in Northern Regions of Bangladesh
by Md. Khokon Miah Akanda ★ , Razia Sultana , Md. Masud Rana , Md. Alamgir Hossain, S. M. Abdul Barik , Md. Rafiul Islam , Md. Nazmul Islam , G.M. Masud Parvez ★
Academic editor: Constancy Prisca Aleru-Obogai
Sciences of Pharmacy 3(1): 24-34 (2024); https://doi.org/10.58920/sciphar0301191
This article is licensed under the Creative Commons Attribution (CC BY) 4.0 International License.
24 Nov 2023
06 Jan 2024
11 Jan 2024
14 Jan 2024
Abstract: In Bangladesh, fungus-related skin diseases are highly prevalent. Until this result began, there was no research in Bangladesh to find the cause and management strategies for fungal infection, but there is still no complete research on it. This survey aimed to evaluate the incidence, etiology, and therapeutic alternatives for various fungal ailments in Bangladesh. The research was carried out in Rajshahi from January to June 2019 by the Pharmacy Department of Varendra University. A compilation of 489 patient data was obtained throughout the investigation using a semi-structured questionnaire. The participants' ages vary from three months to seventy years; 327 are male, and 162 are female. The most prevalent skin conditions among the patients are as follows: ringworm (11.25%), skin infections affecting the ear, nose, fingers, and uterus (11.04%), acne (8.19%), allergy (9.82%), dandruff (5.11%), dermatitis (9.00%), eczema (5.73%), and scabies (7.18%). Student individuals comprise 49.28% of the patients, day workers 16.56%, housewives 16.36%, and employed 14.31%. Patients are housed in 53.17 percent concrete houses, 26.5 percent huts, and 26.18% semi-structures. Patients wash their clothing with tap water at a rate of 52%, followed by tube well water at 21.27%, pond water at 20.45%, and river water at 5.52%. It is evident from this study that fungal diseases affect individuals of all ages, including men and women. An adverse finding of the research was that over forty percent of patients do not receive accurate instructions from their physicians, which raises the risk of drug resistance and further contamination.
Keywords: Fungal diseaseFungal disease prevalenceFungal disease causeFungal disease management
Introduction
A number of skin diseases may be markers of systemic diseases because the skin is the biggest organ in the human body. Skin diseases exhibit a notable prevalence in terms of morbidity, although they appear to have a relatively low incidence of mortalities. Currently, the prevalence of systemic fungal infections poses a significant challenge in both developed and developing countries. Fungal infections affecting the skin and nails have emerged as a prevalent type of infection in recent decades, with an estimated impact on approximately 20-25% of the global population (1). While there has been a significant decrease in the prevalence of fungal diseases in wealthy nations (2-3), several countries in sub-Saharan Africa (4-5) and certain regions of Asia (6-7) continue to bear a high burden of these and other fungal infections. Nevertheless, intensivists in tropical developing nations such as Bangladesh encounter significant challenges when managing an increasing number of fungal infections. Fungal species exhibit wide distribution in soil, plant detritus, and various organic substrates, showcasing their ability to thrive in adverse conditions. They constitute around 7% (611,000 species) of all eukaryotic species on Earth (8). However, only a relatively small proportion of about 600 species has been identified as causing human diseases (9).
Diseases that affect the human skin due to pathological changes, including genetic, inflammatory, benign and malignant, endocrine, hormonal, traumatic, and degenerative processes, are considered skin diseases. Jha et al. revealed that skin diseases had seasonal variations and were statistically significant among outpatient visits in Nepal (10). Dogra S et al. attribute overcrowding and inadequate hygiene to population skin problems (11). The distribution of skin problems varies by country and region. Patients may not seek dermatological condition treatment unless their symptoms are severe due to a lack of awareness. Environment, climate (humidity, temperature), lifestyle (unhygienic), outdoor activities, migration, land usage, economy, literacy, and racial and social conventions also affect skin problems (12-13). Skin disease causes vary by age, sex, and time.
This study draws inspiration from successful international research efforts emphasizing the significance of targeted investigations in understanding and managing fungal diseases. For instance, a study in Bangladesh highlighted that approximately 25% of tannery workers suffer from dermatological diseases (14). Similarly, research in South Korea documented an increase in the prevalence of fungal infections from 6.9% in 2009 to 7.4% in 2013 (15). Comparable studies conducted in countries such as Singapore, Palestine, Nigeria, Algeria, India, Brazil, South Africa, Italy, France, the USA, Canada, and Australia (16-17) have yielded valuable insights into the prevalence, causes, and management strategies for fungal diseases. However, a comprehensive investigation of this nature is lacking within the context of Bangladesh.
Expanding on the methodologies and discoveries from these global studies, this research aims to illuminate the prevalence of various fungal diseases in Bangladesh, consider lifestyle-related factors (such as living conditions, water sources, etc.), and explore effective management strategies, including treatment options. By integrating insights from these global studies, we seek to develop a comprehensive understanding of fungal infections within our region and formulate practical approaches for their management.
Experimental Section
Setting and Design
A prospective study was conducted during the months January to June 2019 in the Rajshahi division. This study was conducted by Department of Pharmacy, Varendra University, Rajshahi. A semi-structured questionnaire was designed and the survey team was guided by the principal investigator G. M. Masud Parvez before the study. The survey group comprised of 8 members. The Survey was done on outdoor patients receiving treatment from the hospitals. A total of 489 patients are collected during the study (18-19).
Data Collection
Patients' data were acquired by randomly picking patients from hospitals, pharmacies, and visiting the patient. The data collectors stationed themselves outside the hospital or pharmacy doors and successfully persuaded patients suffering from fungal infections to disclose their prescription information to the interviewers, facilitating their participation in the interview session. The research conducted in the Rajshahi division of Bangladesh was to investigate the occurrence of fungal diseases. The primary objective was to gather survey data to determine the incidence of these diseases, identify their underlying causes, and gain insights into the existing methods employed for their management. The questionnaire was written in English, which data collectors then translated into Bengali for individuals whose native language is Bengali. During this investigation, a written agreement was obtained from each participant. During the data analysis, some surveys were eliminated due to inadequate information. The inclusion criteria encompass region residents who have experienced or observed fungal diseases, providing valuable insights into prevalence, causes, and management and agree to use for public data by ensuring their privacy. Conversely, the exclusion criteria rule out non-residents, individuals with incomplete survey responses, duplicate entries, and, depending on the focus of the study, either minors or adults who do not agree to use public data and ensure that the data is relevant, accurate, and specific to the study's objectives (20-21).
Statistical Analysis
The acquired data was subjected to descriptive statistical analysis using Microsoft Excel 2013 software.
Ethical Considerations
The study adhered to the ethical principles of the World Medical Association's Declaration of Helsinki (Ref: VU/Pharm_REC: 07_12_2023), approved by the institutional ethics committee. Participants did not use harmful substances, and no samples were collected from them, aligning with ethical guidelines for human subjects in interview-based research.
Result
Basic Patient Characteristics
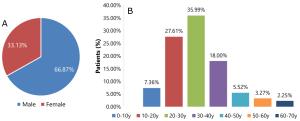
Most patients, particularly those aged 20-30 years, are more susceptible to skin diseases. Males show a higher incidence than females (Figure 1 (A) and Figure 1 (B)). These patients suffer from various skin conditions, including acne, allergy, dandruff, dermatitis, eczema, ringworm, scabies, itching, and infections affecting various body parts. Some patients also exhibit psoriasis, tinea (pedis, vulgaris, cruris), inflammation, and freckles.

Figure 1. Distribution of patients’ gender (A) and age (B). Note: y means years.
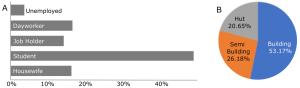
Usually, students suffer the most from fungal infections. At the same time, other professionals such as housewives, job holders, day workers (such as rickshaw puller, farmer, salesman etc.), and unemployed people are also affected (Figure 2 (A)).
Table 1. Pattern of skin disease suffered by patients.
|
Disease |
Frequency |
Percentage |
|
Mycosis (ear, lip, nail, scrotum, skin) |
9 |
1.84% |
|
Acne |
43 |
8.79% |
|
Allergy |
48 |
9.82% |
|
Dandruff, Hair fall |
25 |
5.11% |
|
Dermatitis |
44 |
9.00% |
|
Eczema |
29 |
5.93% |
|
Ringworm |
55 |
11.25% |
|
Scabies |
39 |
7.98% |
|
Itching |
30 |
6.13% |
|
Psoriasis |
11 |
2.24% |
|
Nail abscess |
8 |
1.63% |
|
Candidiasis |
19 |
3.89% |
|
Infection (eye, finger, lip, nail, skin, ear, nose, uterine) |
54 |
11.04% |
|
Tinea (pedis, vulgaris, cruris) |
12 |
2.45% |
|
Inflammation (skin, cervix, vagina) |
13 |
2.66% |
|
Rhinitis |
2 |
0.41% |
|
STD |
8 |
1.63% |
|
Dry skin |
8 |
1.63% |
|
Freckle |
11 |
2.24% |
|
Crack on foot and lips |
2 |
0.41% |
|
Other |
19 |
3.89% |
|
Total |
489 |
100% |
Based on housing data, it is noteworthy that over fifty percent of the population resides in concrete houses, while approximately twenty-five percent of the people live in semi-buildings. Additionally, roughly one-fifth of the population inhabits huts, as depicted in Figure 2 (B). This distribution underscores the diverse nature of housing preferences within the community.

Figure 2. Occupation of patient (A) and accommodation of patient (B).
Prescription Characteristics
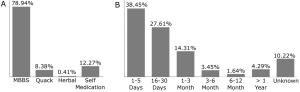
Many patients visited the MBBS doctor for recovery from fungal disease. However, more than 20% of patients take consultation from quack doctors, or they were taking medication as self-medication (Figure 3 (A)).
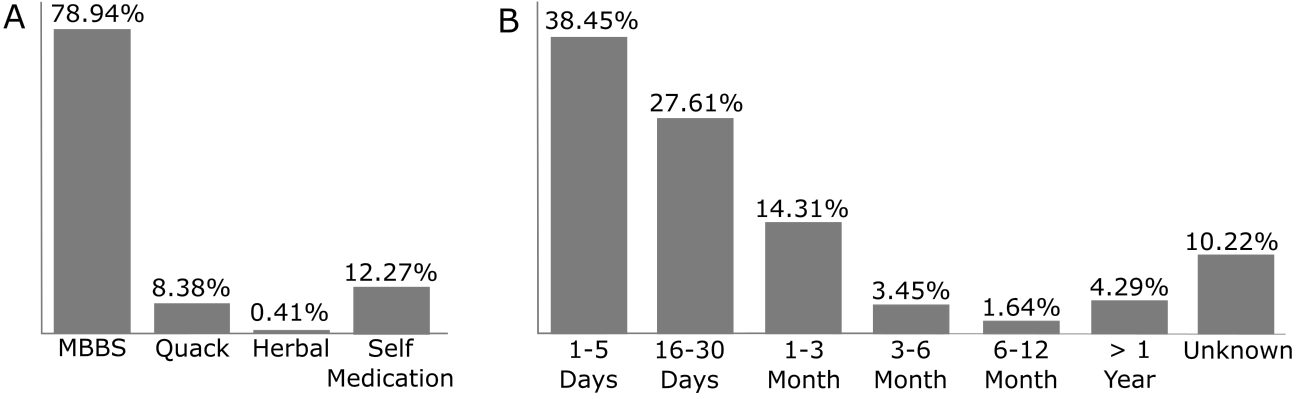
Figure 3. Prescription source (A) and duration of taking medication (B).
The patients were not used to the therapy for a long duration, mostly below one month. Interestingly, about 12% of patients have no clear idea about their treatment, which indicates the careless character of the patients (Figure 3 (B)).
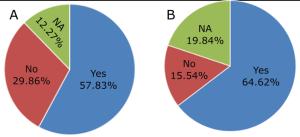
About fifty-eight percent of patients have gotten proper direction from physicians about how to take or use the prescribed drugs, and almost sixty-five percent have gotten sufficient advice from doctors, such as modification to their lifestyle and validation of certain foods (Figure 4 (A), 4 (B)).

Figure 4. Direction of therapy (A) and advice from the doctor (B).
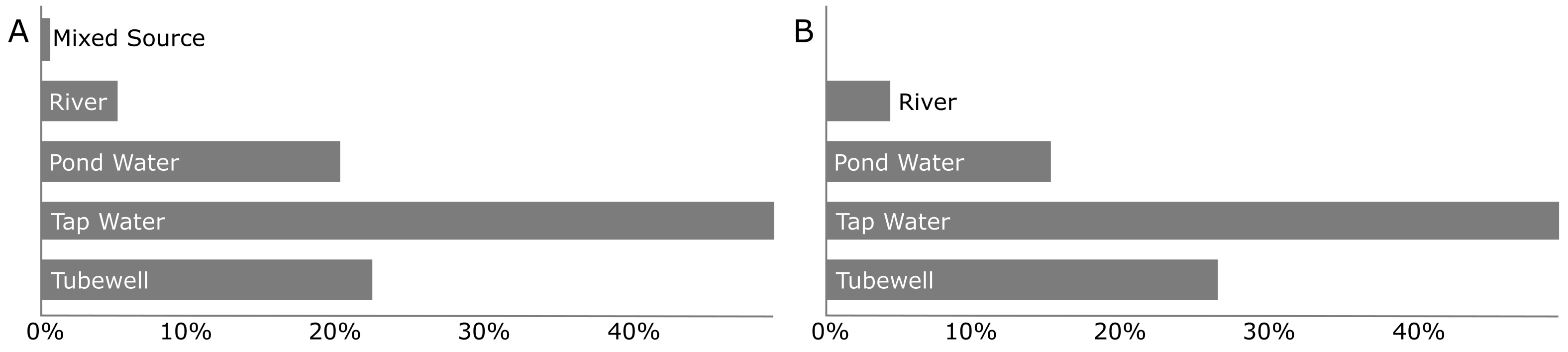
Figure 5. Washing water source (A) and bathing water source (B).

Figure 6. Bed shared by the patient with someone (A) and source of cloth drying (B).
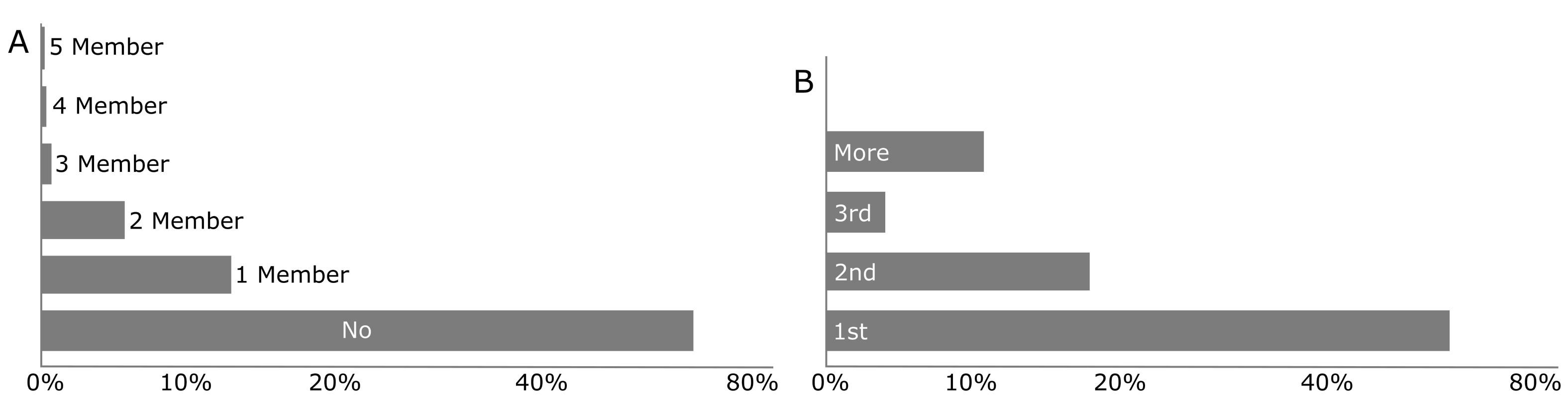
Figure 7. Family members of patients suffering from skin disease (A) and prevalence of disease in each patient (B).
Patient Lifestyles
Patients primarily use tap water for washing clothes, with tubewell and pond water also being notable sources (Figure 5(A)). Tap water is used to a similar extent for taking showers, slightly less with pond water, and more with tubewell water, suggesting a higher preference for tubewell water for bathing over washing clothes (Figure 5(B)).
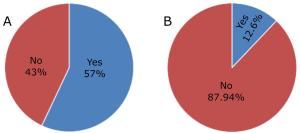
It has been found that more than 40% of patients share their bed with someone responsible for spreading the disease, as fungal infections are contagious (Figure 6 (A)). About ninety percent of patients dry their clothes in sunlight, which is very helpful for killing fungi and curing disease (Figure 6(B)). The rest of the patients use air drying for clothes.
Therapy and Effects
About two-thirds of the patients suffer from fungal disease in their first prevalence, and one-third suffer more than once (Figure 7(A)). It is also observed that more than three-fourths of the patient's family members are safe as they are not suffering from fungal disease (Figure 7(B)).
Corticosteroids, imidazoles, antihistamines, triazoles, scabicides, anti-acne, and various types of antibiotics, such as macrolides, quinolones, cephalosporins etc., treat the patients. Different other drugs like griseofulvin, urea, and paraffin are also used. Vitamins are sometimes given with antibiotics to make up for beneficial bacterial growth. Most of the patients did not observe any side effects, but skin rash (4.91%), drowsiness (3.88%), and nausea (3.27%) were observed.
Discussion
A total of 489 patients were collected from different hospitals and pharmacy shops in Rajshahi city from January to June 2019. It was found that 35.99% of patients were 20-30 years old, 27.61% of patients were 10-20 years old, and 18% were 30-40 years old (Figure 1 (A)). A similar result was found by Mishra et al., which shows that 32.7% of patients are 21-30 years old, and 23.7% are 11-20 years old (22-23). Another study in Bangladesh conducted in Comilla Medical College Hospital found that the age of patients with fungal disease was 24.8% of patients were 10-20 years, 31.1% were 21-30 years, and 15% were 31-40 years old (24). Males are more affected by skin disease and comprise 66.87%, about two-thirds of all the patients (Figure 1 (B)). Ringworm affects 11.25% of patients, followed by infections, mainly on the eye, finger, lip, nail, skin, ear, nose, and uterus. On the other hand, 8.79% of people have acne, 9.82% have allergies, 5.11% have dandruff, 9.00% have dermatitis, 5.93% have eczema, 7.98% have scabies, and 6.13% itch. Similar results were found in previous studies where the fungal infection was the significant skin disease (22), and psoriasis, dermatitis, and scabies were the supreme fungal disease (23, 25-26). In their study, Ahammed et al., found that fungal infection affects 13%, acne 4.8%, and scabies 16.1% of patients in Bangladesh (24). Another study conducted at Faridpur Medical College Hospital, Bangladesh, found that fungal infections affect 17.26% of patients (27). Devi et al. surveyed in North Eastern India and found that the most common skin diseases were eczema (17.48%), fungal infections (17.19%), pyoderma (9.1%), and scabies (8.97%) (28). In another study in 2014-15 in India, it was found that the most commonly encountered diseases were contact dermatitis (11.7% of patients), scabies (8.9%), fungal infections (8.9%), urticaria (6.0%), acne (4.4%) which was quite similar to our study (29). Most skin disease patients are students, which may be due to their living style, such as living close to others, sharing their clothes, etc. The students comprise 49.28%, day workers 16.56%, housewives 16.36%, and job holders 14.31% (Figure 2 (A)). A previous Comilla Medical College Hospital study found that 43.2% of patients are students, 12.5% are housewives, and 11.8% are job holders, which is close to our data (24). However, dermatophytosis, a fungal infection that affects the skin, often affects students. This is especially prevalent in dormitories due to close quarters and shared facilities. Prevention strategies include maintaining good personal hygiene and avoiding sharing personal items like towels and footwear (44).
Housewives are particularly susceptible to fungal infections due to increased exposure to moisture and heat, especially during household tasks. Conditions like tinea manuum (fungus affecting the hands) and tinea pedis are common. They also get scabies because they clean beds and pillows, which are good media for the Sarcoptes scabiei. Preventive measures include minimizing prolonged exposure to water and heat, wearing protective gloves during household tasks, and practicing good skin care. Treatment typically involves topical antifungals (45). Healthcare workers face life-threatening nosocomial fungal infections, requiring strict hygiene, PPE, and environmental controls.
Treatment depends on the specific infection and may involve systemic antifungal therapy (see Table 2). Day workers in construction or agriculture face fungal infections like sporotrichosis due to exposure to contaminated materials. Prevention consists of wearing protective clothing and promptly cleansing skin. Treatment typically involves antifungal agents (46). The distribution of housing types among the patients is as follows: 53.17% reside in concrete houses, 20.65% in huts, and 26.18% in semi-buildings (see Figure 2(B)). Concrete houses are prone to fungal infections due to conditions that favor fungal growth. Fungi like Fusarium can cause significant concrete deterioration by interacting with its calcium content, forming soluble calcium organic complexes, leading to structural weakening. Possible solutions may be improved ventilation control, bio-based self-healing concrete using fungi, high pH adhesive mortars, and antifungal calcite-forming bacteria (47).
It is a positive sign that 78.94% of patients consult with doctors for prescriptions, but 12.27% still take medication without concern from physicians. Quack doctors are also prescribing; their proportion is 8.38% (Figure 3(A)). The patients take the medicines for 1-15 days 38.45%, 16-30 days 27.61% and 1-3 months 14.31% (Figure 3(B)). The study indicated that 57.83% of patients only receive sufficient guidance regarding the usage of required drugs, which raises the likelihood of developing resistance to specific medications. The study also reveals that 64.32% of patients were getting advice from physicians about preventive measures such as how they will live and minimize the chance of further spread of disease or to avoid certain foods to reduce allergic reaction or histamine release (Figure 4 (A), (B)).
Table 2. Therapeutic classification of prescribed drugs.
|
Therapeutic Class |
Drug |
Frequency |
Total Number |
|
Corticosteroids |
Betamethasone valerate |
26 |
91 |
|
Clobetasol propionate |
25 |
||
|
Triamcinolone acetonide |
13 |
||
|
Hydrocortisone 1% |
16 |
||
|
Hydrocortisone acetate |
11 |
||
|
Imidazoles |
ketoconazole |
52 |
172 |
|
Miconazole nitrate |
42 |
||
|
Econazole nitrate 1% |
37 |
||
|
Clotrimazole |
41 |
||
|
Antihistamines |
Levocetirizine dihydrochloride |
10 |
92 |
|
Chlorpherimine maleate |
59 |
||
|
Fexofenodine hydrochloride |
5 |
||
|
Cetirizine dihydrochloride |
15 |
||
|
Rupatadine |
3 |
||
|
Triazoles |
Fluconazole |
78 |
89 |
|
Itraconazole |
11 |
||
|
Pediculicide/ scabicidal |
Permethrin 1% |
44 |
67 |
|
Crotamiton |
23 |
||
|
Anti-acne |
Adapalene |
30 |
40 |
|
Salicylic acid |
10 |
||
|
Bacteriostatic antibiotic |
Fusidic acid |
50 |
50 |
|
Beta-lactam antibiotic |
Flucloxacillin |
15 |
15 |
|
Macrolides |
Azithromycin |
26 |
47 |
|
Erythromycin |
4 |
||
|
Erythromycin |
17 |
||
|
Quinolones/Fluoroquinolone |
levofloxacin |
3 |
5 |
|
Moxifloxacin |
2 |
||
|
Cephalosporins |
Cefuroxime |
3 |
3 |
|
Lincosamide |
Clindamycin |
3 |
3 |
|
Anthelmintics |
Albendazole |
22 |
28 |
|
Mebendazole |
6 |
||
|
Others |
Griseofulvin |
5 |
67 |
|
Metronidazole |
3 |
||
|
Urea |
5 |
||
|
Light paraffin |
6 |
||
|
Olive oil soap |
11 |
||
|
Cleansing soap |
9 |
||
|
Vitamin |
28 |
More than fifty percent of patients use tap water or municipal supply water for washing clothes and households, while tubewells and pond water are used for about 21.27% and 20.45%. About 5.52% of patients use river water for washing (Figure 5(A)). The source of taking a shower shows that tap water is the first choice for most patients, consisting of 51.33%. Tubewell is the second choice, comprising 27.61%, and the third choice is pond water, which is 15.75% (Figure 5(B)). Tap and groundwater may contain fungi like Aureobasidium melanogenum and Candida parapsilosis, potentially contaminating household appliances influenced by calcium, magnesium, and nitrate concentrations. Pond and river water in rural areas is at risk of pathogen contamination, including fecal bacteria and harmful fungi, due to population density and unsanitary latrine practices (36).
Fifty-seven percent of patients share their bed with others (Figure 6 (A)), about 88% of patients use sunlight for drying clothes, and 43% of patients use air drying (Figure 6(B)). Various factors can influence the risk of fungal infection due to sharing beds. For example, in vulnerable populations like migrants or homeless individuals, sharing beds and limited access to laundry facilities increase the risk of foot infections like tinea pedis. Sunlight, which has disinfectant properties, can be beneficial in reducing fungal contamination in clothes (37).
Table 3. Side effects observed by the patient.
Side effect | Frequency | Percent |
Abdominal discomfort | 1 | 0.20% |
Burning sensation | 2 | 0.41% |
Constipation | 3 | 0.61% |
Diarrhea | 1 | 0.20% |
Drowsiness | 19 | 3.88% |
Dry skin | 2 | 0.41% |
Fatigue | 1 | 0.20% |
Fever | 2 | 0.41% |
Food indigestion | 1 | 0.20% |
Headache | 3 | 0.61% |
Itching | 5 | 1.02% |
Irritation | 6 | 1.23% |
Nausea/Vomiting | 16 | 3.27% |
Skin rash | 24 | 4.91% |
Rough skin | 3 | 0.61% |
Sedation | 10 | 2.04% |
Vertigo | 4 | 0.82% |
Weakness | 7 | 1.43% |
No side effect | 379 | 77.51% |
Total | 489 | 100% |
About 66% of patients have experienced fungal disease for the first time (Figure 7(A)), and 10.43% have had fungal infection more than 3 times. Recurrent fungal infections can be attributed to genetic susceptibility, treatment challenges, and immunological deficiencies. Individuals with genetic predispositions, such as those with CARD9 mutations, are more susceptible to these infections due to immune dysfunction. Treatment challenges and recurrence factors can be linked to suboptimal drug bioavailability and lack of effective preventive measures (38). In this study, a positive result is that 76.69% of patients' family members are not suffering from any fungal disease (Figure 7(B)), and in 13.50% of patients, one of their family members suffers. Familial fungal infections are influenced by shared water sources, household practices, environmental and socioeconomic factors, work-from-home dynamics, and clothes drying methods. Shared water sources and shared washing practices contribute to fungal growth, while environmental conditions and socioeconomic factors influence susceptibility and management. Work-from-home dynamics increase close contact, leading to contamination. Clothes drying methods, such as sunlight exposure, reduce fungal contamination. Preventive measures, such as improved hygiene practices, adequate drying, and minimizing personal item sharing, are crucial to reduce transmission within families.
The patients are treated mainly with antifungals, antihistamines, and antibiotics. Similar result was found in previous studies (30-32). The prescription contains imidazole (ketoconazole, miconazole nitrate, econazole nitrate 1%, clotrimazole) highest amount and it is present in 172 prescriptions are used to treat fungal infections such as athlete's foot, jock itch, ringworm, and yeast infections. The second most available drug is antihistamines (92 prescriptions) to relieve allergic symptoms like itching and rashes associated with the fungal infection. The prescribed antihistamines are levocetirizine dihydrochloride, chlorpheniramine maleate, fexofenadine hydrochloride, cetirizine dihydrochloride and rupatadine. The third most available drug is corticosteroids used in fungal diseases to reduce inflammation and suppress immune responses, which can alleviate symptoms, and its number is 91. Betamethasone valerate, clobetasol propionate, triamcinolone acetonide, hydrocortisone 1% and hydrocortisone acetate are the prescribed corticosteroids. The following common drug is triazoles, which is present in 89 prescriptions and fluconazole represents the highest individual drug among all the prescribed drugs. Other drugs like scabicide, anti-acne, and antibiotics (macrolides, quinolones, cephalosporins) are prescribed. Drugs like griseofulvin, urea, and paraffin are also used to treat fungal skin infections and certain skin conditions by promoting hydration, moisturizing, and protecting the skin. The patients observed drowsiness 3.88%, nausea 3.27%, and skin rush 4.91%, but most of the patients, 77.51%, did not observe any side effects (Table 3). Ketoconazole and Clotrimazole drugs have found similar side effects in different studies (33-34). Similarly, Costello et al. (2017) conducted a cross-sectional survey on patient perceptions of glucocorticoid side effects, emphasizing the importance of understanding patient experiences with medication (35).
Several strategies may help minimize the fungal disease in Bangladesh. To combat fungal diseases, public awareness campaigns, regulatory measures, accessible healthcare, community health workers, telemedicine, and engagement are essential. These strategies educate the community about the risks of quack doctors and self-medication, reduce reliance on these practices, and promote hygiene education. Additionally, educating individuals about sharing bedding, isolating infected individuals, encouraging sun drying, and involving communities in discussions about hygiene and individual responsibility are also crucial. Natural foods and supplements can help support the immune system and prevent fungal diseases. Garlic, probiotics, turmeric, coconut oil, oregano oil, vitamin D, zinc, echinacea, ginger, and a balanced diet can help prevent fungal infections (39-43). However, these remedies should not replace medical treatment, and patients should be consulted with a healthcare professional for proper diagnosis and treatment plan.
The study has several limitations. The first limitation of the study is that the data were collected only from Northern regions of Bangladesh. These data do not include areas all over the country. Therefore, regional variation may occur. Secondly, data was not collected throughout the year so seasonal variations may occur. Thirdly, the data in question was derived from the primary diagnoses made by medical professionals. Finally, the patient's age is provided by the patient but not checked from their national identification card.
Conclusion
The increasing incidence of fungal infections over the past two decades is a significant cause of severe infections, leading to increased morbidity and mortality. Factors such as warm and humid climates, poor socioeconomic status, nutritional deficiencies, and overcrowded living conditions contribute to the high rate of fungal and parasitic illnesses. This highlights the need for targeted interventions to improve living conditions and address socioeconomic disparities. The study provides insights into the impact of patients' occupation, housing conditions, water usage, and lifestyle on fungal infection prevalence, marking a significant step forward in understanding the socio-environmental determinants of fungal infections. The research also offers valuable data on the therapeutic classification and side effects of antifungal medications, which is crucial for healthcare professionals in prescribing effective treatments while minimizing adverse effects. The findings lay the foundation for future strategies to reduce fungal infections and improve patient outcomes. Integrating socio-environmental factors with medical interventions is a comprehensive approach to tackling the complex challenge of fungal infections.
Declarations
Acknowledgment
The authors would like to give thanks Professor Dr. Ashik Mosaddik, Department of Pharmacy, Rajshahi University for his cordial support throughout the work.
Ethics Statement
Ethical approval for the study was obtained from the Research Ethics Committee of Varendra University, with the approval number of VU/Pharm_REC:07_12_2023.
Supplemental Material
The raw data collected (cleaned/without patient identity) is available as supplemental data at the link below https://etflin.com/file/document/20231126194951130376736.xlsx
Data Availability
The unpublished data is available upon request to the corresponding author.
Funding Information
Not applicable.
Conflict of Interest
The authors declare no conflicting interest.
References
- Havlickova B, Czaika VA, Friedrich M. Epidemiological trends in skin mycoses worldwide. Mycoses 2008; 51(4): 2–15.
- Dromer F, Mathoulin-Pelissier S, Fontanet A, Ronin O, Dupont B, Lortholary O et al. Epidemiology of HIV-associated cryptococcosis in France (1985–2001): comparison of the pre- and post-HAART eras. AIDS 2004; 18: 555-562.
- Mirza SA, Phelan M, Rimland D, Graviss E, Hamill R, Brandt ME et al. The changing epidemiology of cryptococcosis: an update from population-based active surveillance in 2 large metropolitan areas, 1992-2000. Clinical Infectious Diseases 2003; 36: 789-794.
- Mbanya DN, Zebaze R, Minkoulou EM, Binam F, Koulla S, Obounou A. Clinical and epidemiologic trends in HIV/AIDS patients in a hospital setting of Yaounde, Cameroon: a 6-year perspective. Int J Infect Dis 2002; 6:134-138.
- McCarthy KM, Morgan J, Wannemuehler KA, Mirza SA, Gould SM, Mhlongo N et al. Population based surveillance for cryptococcosis in an antiretroviral-naïve South African province with a high HIV seroprevalence. AIDS 2006; 20: 2199-2206.
- Kong BN, Harwell JI, Suos P, Lynen L, Mohiuddin S, Reinert S et al. Opportunistic infections and HIV clinical disease stage among patients presenting for care in Phnom Penh, Cambodia. Southeast Asian J Trop Med Public Health 2007; 38: 62-68.
- Kumarasamy N, Solomon S, Flanigan TP, Hemalatha R, Thyagarajan SP, Mayer KH. Natural history of human immunodeficiency virus disease in southern India. Clinical Infectious Diseases 2003; 36: 79-85.
- Mora C, Tittensor DP, Adl S, Simpson AG, Worm B. How many species are there on Earth and in the ocean? PLoS Biology 2011; 9:1001-1127.
- Brown GD, Denning DW, Levitz SM. Tackling human fungal infections. Science 2012; 336: 647.
- Jha AK, Gurung D. Seasonal variation of skin diseases in Nepal: A hospital based annual study of outpatient visits. Nepal Medical College Journal 2006; 8:266-268.
- Dogra S, Kumar B. Epidemiology of skin diseases in school children: A study from northern India. Pediatric Dermatology 2003; 20:470-473.
- Rook A, Savin JA, Wilkinson DS. The prevalence, incidence and ecology of diseases of skin, In: Rook A, Wilkinson DS, Ebling FJ, Champion RH, Burton JL, editors, Text book of Dermatology. Oxford University Press: Mumbai 1987. p. 39-53.
- Ungpakorn R. Mycoses in Thailand: current concerns. Nihon Ishinkin Gakkai Zasshi 2005; 46: 818-826.
- Mohanta MK, Saha AK, Hasan MA. Prevalence and determination of occupational diseases of leather tannery workers. University Journal of Zoology Rajshahi University 2012; 31:79-82.
- Yoon HJ, Choi HY, Kim YK, Song YJ, Moran K. Prevalence of fungal infections using National Health Insurance data from 2009-2013, South Korea. Epidemiology and Health 2014; 36:10-17.
- Bongomin F, Gago S, Oladele RO, Denning DW. Global and Multi-National Prevalence of Fungal Diseases-Estimate Precision. J Fungi (Basel) 2017; 3(4):57.
- Soltani S, Zandi M, Faramarzi S, Shahbahrami R, Vali M. et al. Worldwide prevalence of fungal coinfections among COVID-19 patients: a comprehensive systematic review and meta-analysis. Osong Public Health Res Perspect 2022; 13(1): 15-23.
- Akter R, Akanda KM, Islam S, Rana M. Assessment of drug utilization pattern among outpatients in the orthopedic department of several private clinics in Rajshahi city, Bangladesh. International Journal of Pharmaceutical Science and Research 2020; 5(4): 13-16.
- Parvez M, Sultana R, Akanda KM, Mehjabin S, Mosaddik A. Nature and cause of taking psychotropic drugs: a cross-sectional health survey in northern regions of Bangladesh. International journal of Pharmaceutical sciences and research 2018; 9(1): 361-368.
- Sultana R, Akanda KM, Mehjabin S, Parvez M. Prescribing trends of Psychotropic drugs in Northern Bangladesh. Specialty Journal of Medical research and Health Science 2017; 2(2): 17-25.
- Haque MU, Ahmmed SB, Akanda KM, Hasan MT, Mou SA, Sajon SR, Islam A. Prevalence and risk factors of obesity and hypertension among university students in Rajshahi city. Bangladesh pharmaceutical journal 2016; 19(2): 179-184.
- Mishra N, Srivastava N, Gahalaut P, Rastogi MK. Pattern of dermatological disorders in a private skin clinic of Rohilkhand region in India. Journal of Pakistan Association of Dermatologists 2014; 24(2):138-142.
- Renuka A, Purandare CS, Suresh K, Kulkarni AP. Study of Pattern of skin diseases among patients attending OPD of Dermatology, Venereology & Leprosy Department at Bharati Vidhyapeeth Deemed University Medical College & Hospital, Sangli. International Journal of Healthcare and Biomedical Research 2016; 04:30-34.
- Ahammed MA, Haque MJ, Sadir MA, Mortuza SG, Mannan MA. Pattern of Skin Diseases in the In-Patient Department of Comilia Medical College Hospital. Journal of Comilla Medical College Teachers Association 2003; 5(1):1-12.
- Grover S, Ranyal RK, Bedi MK. A cross section of skin diseases in rural Allahabad. Indian Journal of Dermatology 2008; 53(4):179-181.
- Agarwal S, Sharma P, Gupta S, Ojha A. Pattern of skin diseases in Kumaun region of Uttarakhand. Indian Journal of Dermatology, Venereology and Leprology 2011;77: 603-604
- Sarkar SK, Islam AKMS, Sen KG, Ahmed ARS. Pattern of Skin Diseases In Patients Attending OPD Of Dermatology Department At Faridpur Medical College Hospital, Bangladesh. Faridpur Medical College Journal 2010; 5(1):14-16.
- Das KK. Pattern of dermatological diseases in Gauhati Medical College & Hospital, Guwahati. Indian Journal of Dermatology, Venereology and Leprology 2003; 69(1):16-18.
- Sirisha NL, Kumar MP, Sowjanya S. Prevalence of skin diseases in a dermatology outpatient clinic in rims, kadapa, a cross-sectional, retrospective study. Journal of Evolution of Medical and Dental Sciences 2015; 4(57): 9903-9909.
- Paramythiotou E, Frantzeskaki F, Flevari A, Armaganidis A, Dimopoulos G. Invasive Fungal Infections in the ICU: How to Approach, How to Treat. Molecules 2014; 19:1085-1119.
- Badiee P, Hashemizadeh Z. Opportunistic invasive fungal infections: diagnosis & clinical management. Indian Journal of Medical Research 2014; 139:195-204.
- Enoch DA, Ludlam HA, Brown NM. Invasive fungal infections: a review of epidemiology and management options. Journal of Medical Microbiology 2006; 55:809–818.
- Boynton TT, Ferneini EM. Antimicrobial pharmacology for head, neck, and orofacial nonbacterial infections. In: Hupp JR, Ferneini EM, editors. Head, Neck, and Orofacial Infections. Elsevier; 2016. p. 164–73.
- Bell AS. Major Antifungal Drugs. In: Taylor JB, Triggle DJ, editors. Comprehensive Medicinal Chemistry II. Elsevier; 2007. p. 445–68.
- Costello R, Patel R, Humphreys J, McBeth J, Dixon WG. Patient perceptions of glucocorticoid side effects: a cross-sectional survey of users in an online health community. BMJ Open. 2017;7(4):e014603.
- Knappett PSK, Escamilla V, Layton A, McKay LD, Emch M, Williams DE, et al. Impact of population and latrines on fecal contamination of ponds in rural Bangladesh. Sci Total Environ. 2011; 409(17): 3174–82.
- Amichai B, Grunwald M, Davidovici B, Shemer A. Sunlight is said to be the best of disinfectants: the efficacy of sun exposure for reducing fungal contamination in used clothes. The Israel Medical Association journal. 2014; 16(7): 431-433 .
- Alves de Medeiros AK, Lodewick E, Bogaert DJA, Haerynck F, Van daele S, Lambrecht B, et al. Chronic and invasive fungal infections in a family with CARD9 deficiency. J Clin Immunol. 2016;36(3):204–9.
- Parvez M, Akanda KM. Foods and Arthritis: An Overview. In; Watson RR, Preedy VR. Bioactive Food as Dietary Interventions for Arthritis and Related Inflammatory Diseases.Second Edition. Academic Press, Elsevier. 2019: 3-22.
- Akanda KM, Hasan AHMN. Characterization of pharmacological properties of methanolic seed and stem bark extracts of Ziziphus mauritiana (BAU Kul) using in-vitro and in-vivo animal (Swiss albino male mice) model. Clinical Phytoscience. 2021; 7(8):1-13.
- Uzzaman S, Akanda KM, Mehjabin S, Parvez M. A Short Review on a Nutritional Fruit: Guava. Open Access: Toxicology and Research. 2018; 1(1): 1-8.
- Afroja S, Falgunee FN, Jahan MM, Akanda KM, Mehjabin S, Parvez M. Antibacterial Activity of Different Citrus Fruits. Specialty Journal of Medical Research and Health Science. 2017; 2(1): 25-32.
- Parvez M, Akanda KM, Karim R, Mehjabin S, Mou SM, Mosaddik A. Comparative Phytochemical Screening and Antimicrobial Evaluation of Different Varieties of Banana (Musa sapientum). International Journal of Innovative Pharmaceutical Science and Research. 2016; 4(4): 372-383.
- Roy M, Karhana S, Shamsuzzaman M, Khan MA. Recent drug development and treatments for fungal infections. Braz J Microbiol. 2023;54(3):1695–1716.
- Smith DR, Guo Y-LL, Lee Y-L, Hsieh F-S, Chang S-J, Sheu H-M. Prevalence of skin disease among nursing home staff in southern Taiwan. Ind Health. 2002; 40(1):54–58.
- Perlroth J, Choi B, Spellberg B. Nosocomial fungal infections: epidemiology, diagnosis, and treatment. Med Mycol. 2007; 45(4):321–346.
- Gu J-D, Ford TE, Berke NS, Mitchell R. Biodeterioration of concrete by the fungus Fusarium. Int Biodeterior Biodegradation. 1998; 41(2):101–109.

 ETFLIN
Notification
ETFLIN
Notification