Antimicrobial Activity of Triterpenoid and Steroidal Cinnamates from Vitellaria paradoxa
by Olusesan Ojo ★ , Mokgadi P. Mphahlele, Edwin M. Mmutlane , Derek T. Ndinteh ★
Academic editor: Samir Chtita
Sciences of Phytochemistry 4(1): 26-32 (2025); https://doi.org/10.58920/sciphy0401293
This article is licensed under the Creative Commons Attribution (CC BY) 4.0 International License.
02 Nov 2024
22 Feb 2025
05 Mar 2025
13 Mar 2025
Abstract: Antimicrobial resistance (AMR) remains a global threat to human health, and its recent burden has necessitated an urgent need for new antibiotics to fight the growing negative impacts of AMR. Vitellaria paradoxa Gaertn. is a medicinal plant used to treat bacterial infections, including diarrhea, tuberculosis (TB), and other respiratory infections in Africa. This study, therefore, assessed the antimicrobial effect and the cytotoxicity of isolated secondary metabolites from the hexane extract of V. paradoxa stem-bark against a panel of bacterial pathogens. After cold maceration, the resulting extract was purified using column chromatography on silica gel. The resazurin-based 96-well plate micro-dilution method was used to assess the antimicrobial activity of the isolated compounds. On further assay, the MTT assay was used to evaluate the cytotoxic effect of compounds on the cervical cancer cell line (HeLa). The column fractionation led to the isolation of 11-hydroxy β-amyrin cinnamate (compound 1), α-amyrin cinnamate (compound 2), and sitosterol cinnamate (compound 3). All the compounds exhibited antibacterial activity against the tested pathogens, with minimum inhibitory concentration (MIC) ranging from 0.0625 – 1.0 mg/mL. Compound 3 showed the highest antibacterial activity against all bacterial strains (MICs; 0.0625 - 0.25 mg/mL). The compounds showed no remarkable cytotoxic properties (IC50; 77.82 ± 10.5 - 82.53 ± 4.07). As far as we know, the results described the antimicrobial activities of compounds 1-3 for the first time. These results provide scientific justification for the traditional uses of V. paradoxa in treating bacterial infections. The highest antibacterial effect of compound 3 highlights its potential as a lead compound.
Keywords: Drug resistanceVitellaria paradoxaAntibacterialCytotoxicity, Sitosterol cinnamate
Introduction
The incessant rise in antimicrobial resistance (AMR) to clinical antibiotics threatens global health (1). Although antibiotics have been described as one of the major world breakthroughs of the 19th century, AMR has virtually recorded almost all clinical antibiotics (2, 3). An alarming case is the development of methicillin-resistant Staphylococcus aureus (MRSA) (4). AMR is one of the leading causes of death, especially in developing countries where access to basic health care is minimal or absent. Alarmingly, the World Health Organization (WHO) highlighted that the death rates due to AMR would, by 2050, reach 10 million and cost economically more than US$ 100 trillion annually if nothing substantial is done to contain AMR. In addition to the problem of drug resistance, the adverse effects of current antibiotics on the host-like hypersensitivity are another challenge. There are cases of hepatotoxicity (5-7). Hence, this calls for lead drug candidates that would be less expensive and less cytotoxic.
Historically, natural products have been a priceless source of pharmaceutical agents for many diseases, particularly infections from pathogenic microorganisms (8, 9). They are the source of numerous widely used medications, like rifamycin and streptomycin, which are used to treat tuberculosis and other related bacterial illnesses (10, 11). Natural plant-based compounds may have unique mechanisms of action as anti-infective medicines (12-14). The species V. paradoxa Gaertn. is a widely used medicinal plant in sub-Saharan Africa. It is locally called ‘Ori’ (Yoruba, Nigeria), ‘Somou’ (Togo), ‘Taanga’ (Burkina Faso), and ‘karate’ (French). In addition to its uses as a principal component in cosmetics, confectionery, and pharmaceuticals, the species has a long history in the treatment of malaria, diabetes mellitus and hypertension (15), hemorrhoids, fever, diabetes, stroke, cough (16), tuberculosis (17), cancer and tumor, and infections (15). Its anticancer, anti-inflammatory (18), antidiarrheal, and insecticidal properties have all been documented. Previous phytochemical analysis identified rutin, gallic acid, and ferulic acid (15). In our continuous effort to search for lead antimicrobial compounds from natural sources, we isolated three antimicrobial triterpenoid and steroidal cinnamates from the hexane stem-bark extract of V. paradoxa. As far as we are aware, this is the first investigation into the pharmacological action of these compounds against the bacterial pathogens.
Materials and Methods
General Instrumentation
A Brucker Avance III NMR spectrometer was used to analyze the compounds' NMR. Tetramethylsilane (TMS) was utilized as an internal standard to record the 1H (frequency; 500 MHz), 13C (frequency; 125 MHz), and 2D-NMR spectra of the isolated compounds. Additionally, d-CHCl3, or deuterated chloroform, was used as the solvent for the NMR analysis. A Brucker Compact mass spectrometer (University of the Witwatersrand, South Africa) was used to perform and record mass spectra. The Perkin Elmer FTIR 600 series was used for the IR analysis. A column measuring 3 cm by 55 cm filled with silica gel (mesh size: 60–120) was used for column chromatography. Pre-coated silica gel 60 F254 plates (Macherey-Nagel GmbH & Co. KG) with a layer thickness of 0.20 mm were used for thin-layer chromatography (TLC) analysis. The plates were exposed to UV light at 254 and 365 nm after being treated with the p-anisaldehyde-sulphuric acid reagent. The experiment's chemicals were bought from Sigma-Aldrich in South Africa.
Plant Material Collection and Extraction
A stem-bark sample of V. paradoxa was obtained in September 2019 from the University of Ibadan in Oyo State, Western Nigeria. The plant sample was identified taxonomically by Mr. D. P. O. Esimekhuai, Plant Technologist at the Botany Department, University of Ibadan, Nigeria. The voucher specimen (UIH-22897) was deposited in the same department. The stem-bark sample was thoroughly washed before air-drying for 14 days at room temperature and then milled into fine powder. The fine powder was kept in a sealed polythene bag until further use at room temperature. 500 g of pulverized plant sample was extracted with n-hexane (1 L) at room temperature (5 times) for 24 h. After filtering, the extract was concentrated using a rotary evaporator at 40 °C with a lowered pressure, yielding a yellowish-waxy material.
Column Chromatographic Isolation
Before isolation, 10 g of the crude extract was first dissolved in hexane and pre-adsorbed by silica before loading into the glass column. Fractionated was achieved using gradient elution [starting from hexane (100%), with a 10% increase in chloroform to 100% chloroform] on a silica gel column (3 cm × 55 cm) to yield twelve fractions (VPH 1- VPH 12) based on their thin-layer chromatography (TLC) profiles. Fractions VPH 6 (109.5 mg), VPH 7 (2.20 g), and VPH 10 (220.9 mg) were subjected to further fractionation. Fraction VPH 6 was re-chromatographed on a silica gel column, eluting with hexane-ethyl acetate (1:9 to 0:10) as a mobile phase to yield four sub-fractions VPH 6a-d. The sub-fraction VPH 6a appeared as a white solid substance recrystallized from dichloromethane/methanol to yield compound 1 (11-hydroxy β-amyrin cinnamate, 15.4 mg). Fraction VPH 7 was purified on a silica gel-packed column (mobile phase: hexanes-ethyl acetate 97:3 to 10:90) to give three sub-fractions VPH 7a-c. The sub-fraction VPH 7a yielded compound 2 (α-amyrin cinnamate, 26.2 mg) after recrystallizing from dichloromethane/methanol. Sub-fraction VPH 7b was subjected to further purification to give an additional quantity of α-amyrin cinnamate (9.7 mg). Fraction VPH 10 was chromatographed on a silica gel column (mobile phase: hexanes-ethyl acetate 85:15 to 10:90) to give three sub-fractions VPH 10a-c. Sub-fraction VPH 10c (22.10 mg) after recrystallization from dichloromethane/methanol gave compound 3 (sitosterol cinnamate, 9.6 mg). The structures of compounds 1–3 were unambiguously elucidated based on their obtained spectroscopic and physical data and comparison with available literature.
Compound 1, 11-hydroxy β-amyrin cinnamate: White powder; ESI-MS: [M + H]+ m/z = 573.3100; MF: C39H56O3; soluble in CHCl3; 1H-NMR (500 MHz, δ ppm, CHCl3-d = 7.24 ): 7.64 (d, 1H, J = 15.9 Hz, H− 3'), 7.51 (m, 2H, J = 4.2 Hz, H− 6'/8') and 7.50 (1H, H− 7'), 7.35 (d, 2H, J = 4.9 Hz, H− 5'/9'), 6.44 (d, 1H, J = 10.0 Hz, H− 2'), 5.56 (dd, 1H, H− 12), 4.62 (dd, 1H, J = 9.80 and 5.3 Hz, H− 3), 4.10 (t, 1H, J = 3.5 Hz, H− 11), 0.77–1.03 (s, 8×3H); 13C-NMR (125 MHz, δ ppm, CHCl3-d = 77.23 ): 38.75 (CH2, C− 1), 23.96 (CH2, C− 2), 80.85 (CH, C− 3), 37.09 (C, C− 4), 55.58 (CH, C− 5), 18.51 (CH2, C− 6), 32.17 (CH2, C− 7), 42.32 (C, C− 8), 47.92 (CH, C− 9), 39.89 (C, C− 10), 81.27 (CH, C− 11), 124.59 (CH, C− 12), 139.88 (C, C− 13), 42.35 (C, C− 14), 26.87 (CH2, C− 15), 28.37 (CH2, C− 16), 33.15 (C, C− 17), 59.34 (CH, C− 18), 41.79 ( CH2, C− 19), 31.50 (C, C− 20), 34.00 (CH2, C− 21), 40.31 (CH2, C− 22), 28.98 (CH3, C− 23), 15.99 (CH3, C− 24), 14.33 (CH3, C− 25), 17.14 (CH3, C− 26), 25.40 (CH3, C− 27), 28.98 (CH3, C− 28), 17.74 (CH3, C− 29), 22.93 (CH3, C− 30), 167.02 (C, C− 1'), 144.48 (CH, C− 2'), 119.13 (CH, C− 3'), 134.84 (C, C− 4'), 128.26 (CH, C− 5'/9'), 129.07 (CH, C− 6'/8'), 130.33 (CH, C− 7'). These data are consistent with those reported in the literature for 11α-hydroxy-β-amyrin by Ikuta and Morikawa (19) and its cinnamate by Sirignano et al. (20).
Compound 2, α-amyrin cinnamate: White solid powder; ESI-MS: [M + H]+ m/z = 557.4117; MF: C39H56O2; m.p = 231–235 (uncorrected); soluble in CHCl3; 1H-NMR (500 MHz, δ ppm, CHCl3-d = 7.24 ): 7.64 (d, 1H, J = 16.0 Hz, H− 3'), 7.52 (m, 2H, J = 3.95 Hz, H− 6'/8') and 7.50 (1H, H− 7'), 7.35 (d, 2H, J = 4.15 Hz, H− 5'/9'), 6.42 (d, 1H, J = 16.0 Hz, H− 2'), 5.76 (dd, 1H, H− 12), 4.61 (dd, 1H, J = 9.80 and 6.30 Hz, H− 3), 0.76–1.20 (s, 8×3H); 13C-NMR (125 MHz, δ ppm, CHCl3-d = 77.23 ): 38.72 (CH2, C− 1), 23.61 (CH2, C− 2), 81.22 (CH, C− 3), 37.05 (C, C− 4), 55.54 (CH, C− 5), 18.49 (CH2, C− 6), 33.11 (CH2, C− 7), 40.27 (C, C− 8), 47.88 (CH, C− 9), 38.17 (C, C− 10), 23.93 (CH2, C− 11), 124.55 (CH, C− 12), 139.84 (C, C− 13), 42.31 (C, C− 14), 26.84 (CH2, C− 15), 28.33 (CH2, C− 16), 33.96 (C, C− 17), 59.30 (CH, C− 18), 39.83 (CH, C− 19), 39.88 (CH, C− 20), 31.48 (CH2, C− 21), 41.76 (CH2, C− 22), 28.36 (CH3, C− 23), 17.10 (CH3, C− 24), 15.97 (CH3, C− 25), 17.13 (CH3, C− 26), 23.47 (CH3, C− 27), 28.97 (CH3, C− 28), 17.72 (CH3, C− 29), 21.61 (CH3, C− 30), 166.97 (C, C− 1'), 144.46 (CH, C− 2'), 119.08 (CH, C− 3'), 134.79 (C, C− 4'), 128.23 (CH, C− 5'/9'), 129.03 (CH, C− 6'/8'), 130.30 (CH, C− 7'); FTIR (KBr) υmax: 2854.2, 2933.3 (C-H, aliphatic), 1706.9 (C = O), 1634.1 (C = C) cm− 1. These findings correspond with those published in the literature for α-amyrin cinnamate by (18) and Miranda et al. (21).
Compound 3, sitosterol cinnamate: White powder; ESI-MS: [M + H]+ m/z = 545.8512; Molecular formula: C38H56O2; soluble in CHCl3; 1H-NMR (500 MHz, δ ppm, CHCl3-d = 7.24 ): 7.64 (d, 1H, J = 15.8 Hz, H− 3'), 7.51 (m, 2H, J = 4.2 Hz, H− 6'/8') and 7.50 (1H, H− 7'), 7.35 (d, 2H, J = 4.9 Hz, H− 5'/9'), 6.42 (d, 1H, J = 16.0 Hz, H− 2'), 5.12 (dd, 1H, J = 5.8 Hz, H− 6), 3.57 (dd, 1H, H− 3), 0.77-1.00 (s, 6×3H); 13C-NMR (125 MHz, δ ppm, CHCl3-d = 77.23 ): 38.23 (CH2, C− 1), 29.91 (CH2, C− 2), 71.28 (CH, C− 3), 39.72 (CH2, C− 4), 139.78 (C, C− 5), 119.12 (CH, C− 6), 29.57 (CH2, C− 7), 32.10 (CH, C− 8), 51.48 (CH, C− 9), 34.47 (C, C− 10), 21.79 (CH2, C− 11), 37.40 (CH2, C− 12), 43.53 (C, C− 13), 55.37 (CH, C− 14), 23.25 (CH2, C− 15), 28.71 (CH2, C− 16), 56.17 (CH, C− 17), 12.28 (CH3, C− 18), 19.23 (CH3, C− 19), 40.52 (CH, C− 20), 21.29 (CH3, C− 21), 31.71 (CH2, C− 22), 25.61 (CH2, C− 23), 49.71 (CH, C− 24), 41.01 (CH, C− 25), 13.25 (CH3, C− 26), 21.59 (CH3, C− 27), 22.90 (CH2, C− 28), 12.45 (CH3, C− 29), 167.0 (C, C− 1'), 144.5 (CH, C− 2'), 117.6 (CH, C− 3'), 138.36 (C, C− 4'), 128.25 (CH, C− 5'/9'), 129.06 (CH, C− 6'/8'), 129.06 (CH, C− 7'); FTIR (KBr) υmax: 2854.2, 2920.1 (aliphatic, C-H), 1706.9 (C = O), 1634.1 (C = C), 1165.8 (C-O) cm− 1. Compound 3 is identified as sitosterol cinnamate based on the 1H and 13C-NMR, MS, and FTIR data above and compared with those published in the literature (22).
Antimicrobial Activity
Microbial Strains and Culture
The reference strains of Mycobacterium smegmatis (MC 2155) (which is used as “surrogate” model for the virulent Mycobacterium tuberculosis), Staphylococcus aureus (ATCC 25923), Escherichia coli (ATCC 25922), Klebsiella aerogenes (ATCC 13882), Enterobacter cloacae (ATCC 13047), Enterococcus faecalis (ATCC 13047), and Klebsiella oxytoca (ATCC 8724) were used for the antimicrobial screening. The strains were maintained at -80 °C until use. M. smegmatis strain was cultivated on Middlebrook 7H11 agar under hygienic conditions, supplemented with 10% (v/v) oleic acid, albumin, dextrose, and catalase, and allowed to grow for a day. Middlebrook 7H9 broth was employed to determine the compounds' minimum inhibitory concentrations (MICs) on M. smegmatis. Nutrient agar was used to activate other bacterial strains. The Mueller-Hinton broth was used to assess the MIC values of these strains (23).
Minimum Inhibitory Concentrations (MICs) Determination
MIC was expressed as the lowest concentration of the tested compounds that completely inhibited bacterial growth and irreversibly changed the blue dye of the resazurin solution to pink (24) (Table 1). The antimicrobial activity of the test compounds was evaluated in a 96-well plate using resazurin micro-titre assay against the microbial strains as previously described (23), with minimal adjustment. The solutions of the test compounds were made in dimethyl sulphoxide (DMSO) to afford a concentration of 1.0 mg/mL and diluted (two folds) serially to afford working concentrations from 1.0 to 0.0313 mg/mL in a 96-well plate to 7H9 broth for M. smegmatis, and Mueller-Hinton broth for other bacterial strains. 100 µL of a standardized inoculum suspension (1.5×106 CFU/mL) was used to seed 100 µL of each concentration in duplicate under aseptic conditions. The plates were then sealed and incubated at 37 °C for 24 h. Viable bacterial cells were confirmed calorimetrically by adding resazurin dye (40 µL of 200 µg/mL) after incubating for 2 h at 37 °C, as they enzymatically converted resazurin dye (blue color) to resorufin (pink color), while non-viable cells remained blue. Muller-Hilton broth (50% v/v in DMSO) was used as a negative control. The bacterial growth was not experimentally affected by the DMSO concentration in the well, ensuring reliable results. Two broad-spectrum antibiotics, streptomycin and nalidixic acid, served as positive controls for comparison and validation of antimicrobial activity.
Table 1. Antimicrobial and cytotoxicity of tested compounds 1-3 from Vitellaria paradoxa.
| Antimicrobial (MIC, mg/mL) | Cytotoxicity (IC50 µg/mL) | ||||||
Strains | Ms | Ec | Ka | Sa | Ecl | Ko | Ef | HeLa |
Compound 1 | 0.50 | 0.50 | 0.50 | 0.50 | 0.50 | 0.50 | 0.50 | 82.53± 4.06 |
Compound 2 | 1.00 | 0.50 | 0.50 | 0.50 | 1.00 | 0.50 | 0.50 | 77.82± 10.5 |
Compound 3 | 0.125 | 0.0625 | 0.250 | 0.0625 | 0.0625 | 0.0625 | 0.0625 | Not determined |
Streptomycin | 0.004 | 0.064 | 0.016 | 0.256 | 0.512 | 0.016 | 0.128 | - |
Nalidixic acid | 0.512 | 0.512 | 0.256 | 0.064 | 0.016 | 0.008 | >0.512 | - |
Note: Sa - Staphylococcus aureus; Ec - Escherichia coli; Ecl - Enterobacter cloacae; Ko - Klebsiella oxytoca; Ka - Klebsiella aerogenes; Ms - Mycobacterium smegmatis; Ef - Enterococcus faecalis; HeLa – Human cancer cell line | ||||||||
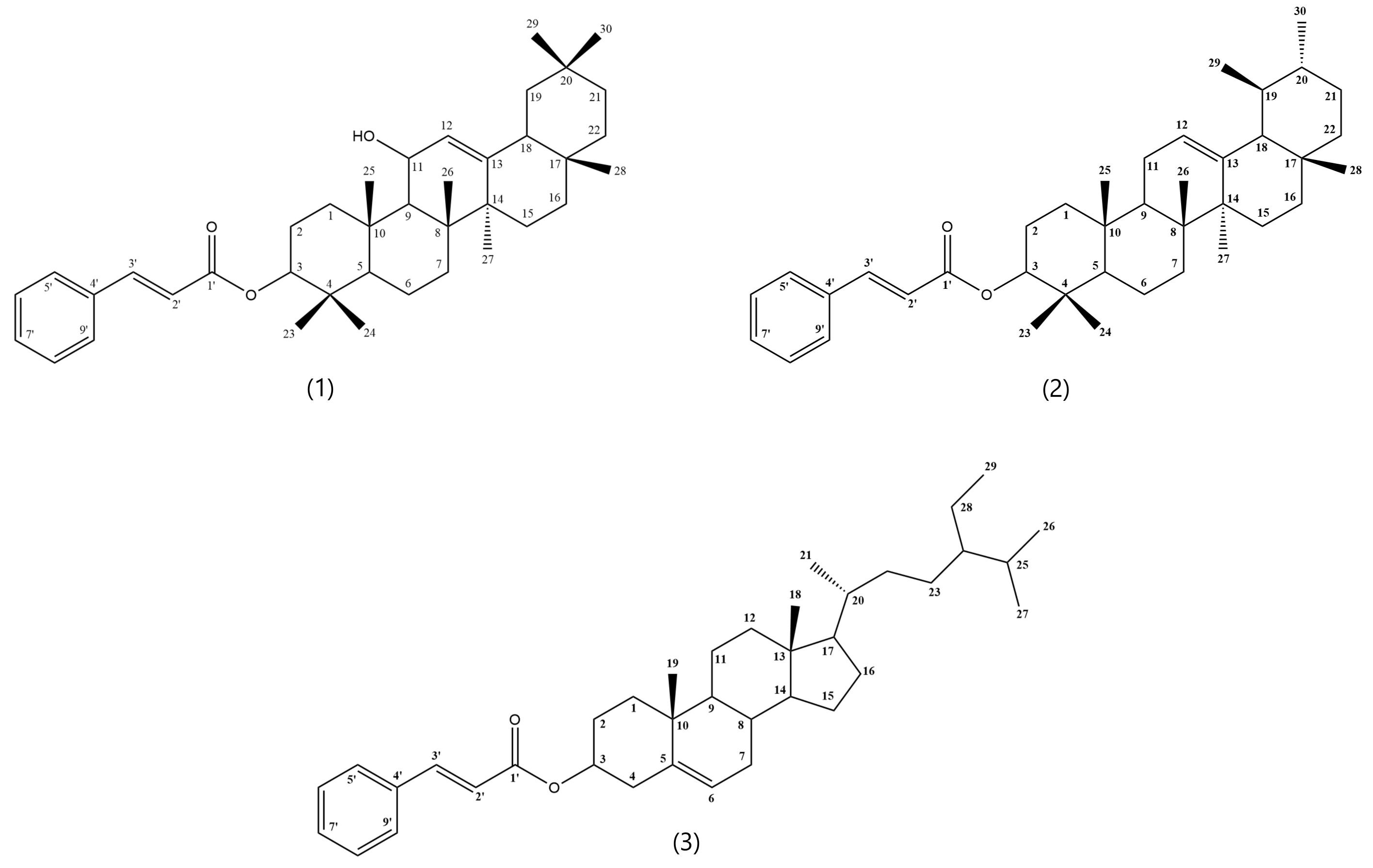
Figure 1. Chemical structures of compounds 1-3 isolated from Vitellaria paradoxa stem-bark.
In Vitro Cytotoxicity
The in vitro cytotoxicity of the compounds was assessed against human cervical cancer cell line (HeLa cells) using MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide, a tetrazole) assay as previously described (25), with minimal adjustment. The stock samples’ concentrations ranging from 62.5 to 1000 µg/mL were made in 100% dimethyl sulphoxide (DMSO) and incubated with HeLa cells in a 96-well plate (1 × 104 cells/mL) cultured and maintained in DMEM with 10% (v/v) fetal bovine serum (FBS) at 37 °C for 1 day in an environment of 5% carbon dioxide. 100 µL of pure DMSO was added to the control cells. By adding a resazurin-based reagent and then measuring the resorufin fluorescence in a multi-well micro-plate reader (VERSAmax, USA) at 595 nm, the number of HeLa cells that survived the exposure of the tested samples was determined. The experiments were duplicated, and a mean standard deviation (SD) was calculated for each. The results were expressed as percentage (%) cell viability based on the fluorescence reading in treated wells compared to control wells (Table 1).
Result and Discussion
In the present study, we report the isolation of antimicrobial compounds from V. paradoxa, a medicinal plant used for treating bacterial infections, including diarrhea and tuberculosis. The hexane extract of the plant stem-bark was subjected to silica gel column chromatography to afford three bioactive compounds, namely 11-hydroxy β-amyrin cinnamate [1] (20), α-amyrin cinnamate [2] (21), and sitosterol cinnamate [3] (22) (Figure 1). The chemical structures of the three compounds were established by thoroughly analyzing their 1H- and 13C-NMR, 2D-NMR, and HR-ESIMS (Provided in Supplementary Material) and comparing them with previous spectroscopic data reported in the literature. To the best of our knowledge, compounds 2 and 3 are reported for the first time in this study from the stem bark of V. paradoxa.
To explore the contribution of compounds 1-3 to the ethnopharmacological uses of V. paradoxa in the treatment of bacterial infections, they were screened against a panel of bacterial pathogens, including Staphylococcus aureus and M. smegmatis (used as study model for M. tuberculosis) (Table 1) using resazurin-based 96-well plate micro-dilution method.
The isolated compounds 1-3 pharmacologically exhibited antimycobacterial activity, with sitosterol cinnamate [3] displaying the best activity against the inhibition of M. smegmatis (MIC; 0.125 mg/mL). Compound 3 showed the best activity against other tested bacterial pathogens, with MICs varying from 0.0625 to 0.25 mg/mL. Compared to one of the positive controls, compound 3 demonstrated superior or comparable action to nalidixic acid against S. aureus, E. coli, M. smegmatis, K. aerogenes, and E. faecalis. Additionally, it showed greater or comparable activity to streptomycin against S. aureus, E. coli, E. faecalis, and E. cloacae.
Convincingly, chemical structure dictates the functions/activity of a compound. Structurally, all the isolates 1–3 (see Figure 1) contain cinnamoyl groups at the C-3 position. It is well-known that many drug-like compounds with increased biological activity, such as antimycobacterial and antimalarial compounds, contain cinnamoyl functionality (26, 27). Presumably, the better activity of compound 3 (tetracyclic steroid-like core) might be related to the structural difference when compared with compounds 1 and 2, which mainly consist of pentacyclic triterpenoid-like core. Meanwhile, in setting clinical benchmark, Gibbons (28) established a clinical benchmark by noting that a plant extract or its natural product has minimal therapeutic significance if its MIC values are higher than 1.0 mg/mL, and based on this criterion, compounds 1–3, therefore, fall in Gibbons' benchmark (28). The presence of compounds 1-3 has previously been reported in V. paradoxa (15), and as far as we know, their antimicrobial activity is being reported for the first time. Interestingly, it should be noted that there is little information regarding the occurrence of compounds 1-3 in plants. These findings lend credence to the widespread ethnobotanical usage of V. paradoxa as an herb to treat diarrhoeal, typhoid fever, cough, tuberculosis, and other bacterial infections.
The anticancer activity of compounds 1 and 2 was tested against the human cancer cell line (HeLa) by conducting an MTT cell viability assay. Isolate 3 could not be evaluated because of its limited quantity. As observed in Table 1, compounds 1 and 2 showed no cytotoxic effect against HeLa cells, as shown from the obtained IC50 values, which were more than 4 µg/mL according to the benchmark established by the American National Cancer Institute (NCI) (29) for plant natural products to be considered cytotoxic. Although in contrast to our study, the in vivo antitumor-promoting effect of compound 2 to inhibit the progression of skin tumors using Epstein-Barr virus early antigen (EBV-EA) in Raji cells has been described (21), this is the first report about the non-cytotoxic effect of 1 against cancer cell line (HeLa cell line). The current study can be improved by using more than one cancer cell line and normal human cell line in an in vitro and in vivo assay to unravel the safety of these compounds as lead antimicrobials in rational drug design and development.
Conclusion
The present study extends the available information on the chemical constituents and bioactivity of V. paradoxa. It offers three compounds that can be explored in the design of antimicrobial agents against bacterial infections. They are 11-hydroxy β-amyrin cinnamate (1), α-amyrin cinnamate (2), and sitosterol cinnamate (3). The compounds showed no remarkable cytotoxic properties (IC50; 77.82 ± 10.5 - 82.53 ± 4.07). The antimicrobial activity of compound 3 (MICs; 0.0625 - 0.25 mg/mL) highlights its potential as a promising bioactive molecule to fight pathogenic bacteria. As far as we know, the results described the antimicrobial activities of compounds 1-3 for the first time.
However, a comprehensive evaluation of the potential harmful effects of these compounds is essential for their successful integration into rational drug design and development. This includes thorough toxicity profiling through in vitro cytotoxicity assays, in vivo pharmacokinetic and toxicological studies, and mechanistic evaluations to identify any adverse effects at the molecular, cellular, and systemic levels. Understanding these risks is crucial to ensure both efficacy and safety, ultimately aiding in refining these compounds as viable therapeutic candidates. Additionally, long-term studies assessing chronic toxicity, potential bioaccumulation, and off-target interactions are necessary to predict their long-term impact. Regulatory compliance and risk-benefit assessments will further facilitate their progression from experimental compounds to clinically approved therapeutics.
Declarations
Acknowledgment
The authors are grateful to the funding organization. The authors acknowledge Chemical Science Department, University of Johannesburg for providing access to research laboratory and facilities.
Ethics Statement
None of the authors performs experiment that involves animals or human. Therefore, ethic clearance is not applicable for this research.
Data Availability
Data used in this study have been included in the manuscript, and available upon request to the corresponding author.
Funding Information
This research work was financially supported by National Research Foundation (NRF), South Africa, with grant number 139057.
Conflict of Interest
The authors declare no conflicting interest.
References
- Christaki E, Marcou M, Tofarides A. Antimicrobial resistance in bacteria: mechanisms, evolution, and persistence. J Mol Evol. 2020;88:26–40. https://doi.org/10.1007/s00239-019-09914-3.
- Cook MA, Wright GD. The past, present, and future of antibiotics. Sci Trans Med. 2022;14:eabo7793. https://doi.org/10.1126/scitranslmed.abo7793.
- Mancuso G, Midiri A, Gerace E, Biondo C. Bacterial antibiotic resistance: the most critical pathogens. Pathog. 2021;10:1310. https://doi.org/10.3390/pathogens10101310.
- Dettweiler M, Melander RJ, Porras G, Risener C, Marquez L, Samarakoon T, et al. A clerodane diterpene from Callicarpa americana resensitizes methicillin-resistant Staphylococcus aureus to β-lactam antibiotics. ACS Infect Dis. 2020;6:1667–73. https://doi.org/10.1021/acsinfecdis.0c00307.
- Dadgostar P. Antimicrobial resistance: implications and costs. Infect Drug Resistance. 2019;12:3903–10. https://doi.org/10.2147/IDR.S234610.
- Zhen X, Lundborg CS, Sun X, Hu X, Dong H. Economic burden of antibiotic resistance in ESKAPE organisms: a systematic review. Antimicrob Resist Infect Control. 2019;8:137. https://doi.org/10.1186/s13756-019-0590-7.
- Shrivastava SR, Shrivastava PS, Ramasamy J. World Health Organization releases global priority list of antibiotic-resistant bacteria to guide research, discovery, and development of new antibiotics. J Med Soc. 2018;32:76. https://doi.org/10.4103/jms.jms_25_17.
- Copp BR, Pearce AN. Natural product growth inhibitors of Mycobacterium tuberculosis. Nat Prod Rep. 2007;24:278–97. https://doi.org/10.1039/B513520F.
- Atanasov AG, Zotchev SB, Dirsch VM, Supuran CT. Natural products in drug discovery: advances and opportunities. Nat Rev Drug Discov. 2021;20:200–16. https://doi.org/10.1038/s41573-020-00114-z.
- Wall ME. Camptothecin and taxol: Discovery to clinic. Med Res Rev. 1998;18:299–314. https://doi.org/10.1002/(SICI)1098-1128(199809)18:5<299::AID-MED2>3.0.CO;2-O.
- Nguta JM, Appiah-Opong R, Nyarko AK, Yeboah-Manu D, Addo PGA. Current perspectives in drug discovery against tuberculosis from natural products. Inter J Mycobacteriol. 2015;4:165–83. https://doi.org/10.1016/j.ijmyco.2015.05.004.
- Waterman C, Smith RA, Pontiggia L, DerMarderosian A. Anthelmintic screening of Sub-Saharan African plants used in traditional medicine. J Ethnopharmacol. 2010;127:755–9. https://doi.org/10.1016/j.jep.2009.11.025.
- Rates SMK. Plants as source of drugs. Toxicon. 2001;39:603–13. https://doi.org/10.1016/S0041-0101(00)00154-9.
- Savoia D. Plant-derived antimicrobial compounds: alternatives to antibiotics. Future Microbiol. 2012;7:979–90. https://doi.org/10.2217/fmb.12.68.
- Ojo O, Kengne MHK, Fotsing MC, Mmutlane EM, Ndinteh DT. Traditional uses, phytochemistry, pharmacology and other potential applications of Vitellaria paradoxa Gaertn. (Sapotaceae): a review. Arabian J Chem. 2021;14:103213. https://doi.org/10.1016/j.arabjc.2021.103213.
- Ariyo OC, Usman MB, Olorukooba MM, Ariyo MO, Suleiman R, Aasa OS, et al. Ethnobotanical survey of medicinal plants used in the treatment of cough in Akinyele Local Government Area, Oyo State, Nigeria. Eur J Med Plants. 2020:101–13. https://doi.org/10.9734/ejmp/2020/v31i830263.
- Ogbole OO, Ajaiyeoba EO. Traditional management of tuberculosis in Ogun State of Nigeria: the practice and ethnobotanical survey. Afr J Tradit Complement Altern Med. 2009;7:79–84. https://doi.org/10.4314/ajtcam.v7i1.57270.
- Akihisa T, Kojima N, Kikuchi T, Yasukawa K, Tokuda H, T. Masters E, et al. Anti-inflammatory and chemopreventive effects of triterpene cinnamates and acetates from shea fat. J Oleo Sci. 2010;59:273–80. https://doi.org/10.5650/jos.59.273.
- Ikuta A, Morikawa A. Triterpenes from Stauntonia hexaphylla callus tissues. J Nat Prod. 1992;55:1230–3. https://doi.org/10.1021/np50087a008.
- Sirignano C, Nadembega P, Poli F, Romano B, Lucariello G, Rigano D, et al. Triterpenoids from Vitellaria paradoxa stem barks reduce nitrite levels in lps-stimulated macrophages. Plants. 2021;10:1006. https://doi.org/10.3390/plants10051006.
- Miranda ALP de, Silva JRA, Rezende CM, Neves JS, Parrini SC, Pinheiro MLB, et al. Anti-inflammatory and analgesic activities of the latex containing triterpenes from Himatanthus sucuuba. Planta Med. 2000;66:284–6. https://doi.org/10.1055/s-2000-8572.
- Buxton T, Takahashi S, Eddy Doh A-M, Baffoe-Ansah J, Owusu EO, Kim C-S. Insecticidal activities of cinnamic acid esters isolated from Ocimum gratissimum L. and Vitellaria paradoxa Gaertn leaves against Tribolium castaneum Hebst (Coleoptera: Tenebrionidae). Pest Management Sci. 2020;76:257–67. https://doi.org/10.1002/ps.5509.
- Kuete V, BetrandTeponno R, Mbaveng AT, Tapondjou LA, Meyer JJM, Barboni L, et al. Antibacterial activities of the extracts, fractions and compounds from Dioscorea bulbifera. BMC Compl and Altern Med. 2012;12:228. https://doi.org/10.1186/1472-6882-12-228.
- Eloff J. A sensitive and quick microplate method to determine the minimal inhibitory concentration of plant extracts for bacteria. Planta Med. 1999;64:711–3. https://doi.org/10.1055/s-2006-957563.
- Parthasarathy R, Shanmuganathan R, Pugazhendhi A. Vinblastine production by the endophytic fungus Curvularia verruculosa from the leaves of Catharanthus roseus and its in vitro cytotoxicity against HeLa cell line. Anal Biochem. 2020;593:113530. https://doi.org/10.1016/j.ab.2019.113530.
- De P, Bedos-Belval F, Vanucci-Bacqué C, Baltas M. Cinnamic acid derivatives in tuberculosis, malaria and cardiovascular diseases - a review. Curr Org Chem. 2012;16:747–68. https://doi.org/10.2174/138527212799958020.
- Tanachatchairatana T, Bremner JB, Chokchaisiri R, Suksamrarn A. Antimycobacterial activity of cinnamate-based esters of the triterpenes betulinic, oleanolic and ursolic acids. Chem Pharm Bull. 2008;56:194–8. https://doi.org/10.1248/cpb.56.194.
- Gibbons S. Anti-staphylococcal plant natural products. Nat Prod Rep. 2004;21:263–77. https://doi.org/10.1039/b212695h.
- Pezzuto JM. Natural compounds in cancer therapy. Pharm Biol. 2002;40:79–79. https://doi.org/10.1076/phbi.40.1.79.5858.

 ETFLIN
Notification
ETFLIN
Notification







