Psychotropic Drugs Used in Psychiatry Outpatient Department: A Cross-Sectional Drug Utilization Research
by Hiteswar Saikia, Mustakim Ahmed, Anju L. Saikia ★ , Daisy Phukan
Academic editor: Pilli Govindaiah
Sciences of Pharmacy 2(3): 148-157 (2023); https://doi.org/10.58920/sciphar02030042
This article is licensed under the Creative Commons Attribution (CC BY) 4.0 International License.
04 Apr 2023
06 Jun 2023
05 Jul 2023
06 Jul 2023
Abstract: Mental and behavioral disorders are common around the world. Pharmacotherapy, psychotherapy, and psychosocial rehabilitation are three treatment components for these disorders. Drug therapy is an essential part of the comprehensive treatment of these diseases. Their use pattern in psychiatric practice has changed dramatically in recent years. Mental disorders require long-term treatment. Therefore, it is crucial to study the prescribing practices of these groups of drugs. This study aims to assess drug use patterns using the WHO/INRUD Core Prescribing Indicators. Patients of both genders and ages with mental illness and prescription psychiatric drugs were evaluated from the outpatient department of the Psychiatry Unit (OPD). The prescription data were collected and analyzed using the indicators recommended by the WHO/INRUD. The data were analyzed using Microsoft Excel-2007. The percentage and average values of the variables were compared. A total of 655 prescriptions were analyzed. Male patients (54.96%) were more than women (45.04%). The morbidity profile included schizophrenia (37.86%), alcohol use disorder (18.78%), major depressive disorder (11.30%), anxiety disorder (10.23%), bipolar disorder (4.88%), and others (16.95%). The newer antipsychotic were the most commonly prescribed drugs (particularly olanzapine), along with a central anticholinergic (trihexyphenidyl) and a benzodiazepine (lorazepam). The percentage of drugs prescribed with generic names was 39.80%, and that of drugs prescribed by NLEM was 48.49%. The average number of drugs prescribed per prescription was 2.58. This study's Index of Rational Prescribing (IRDP) was 3.87, whereas the optimal score was 5. Prescriptions were complete, and principles of rational prescribing were followed, except for a low generic prescribing rate.
Keywords: Drug utilization studyPsychotropic drugsWHO prescribing indicatorsRational drug prescribing
Introduction
Drug utilization research (DUR) is defined by the World Health Organization (WHO,1977) as "the marketing, distribution, prescription, and use of drugs in society, with particular emphasis on the medical, social, and economic consequences". The main goal of drug use research is to facilitate the rational use of drugs in the population. For an individual patient, reasonable drug use means prescribing a well-studied medication at an optimal dose, with correct information, and at an affordable price (1). DUR is important in pharmacoepidemiology due to its close association with- public health, pharmacovigilance, pharmacoeconomics, and pharmacogenetics (2).
Mental disorders are included in the Global Burden of Diseases (3). Epidemiological studies in India indicate an incidence rate of around 18-20 per thousand of the population. Pharmacological therapy, psychotherapy, and psychosocial rehabilitation are the main components of treating mental illness (4). The prescription pattern of psychotropic medication use in psychiatric practice has changed dramatically (5). Many new psychotropic drugs are available to treat mental disorders and have radically changed the therapeutic protocols (6). The rapidly evolving field of psychopharmacology challenges traditional concepts of psychiatric treatment and constantly seeks new and improved drugs to treat these disorders. At the same time, the drugs should also be safer and efficacious (7).
According to the Global Burden of Disease Study 1990–2017 across the states of India, mental disorders included depressive disorders, anxiety disorders, schizophrenia, bipolar disorder, idiopathic development, intellectual disability, conduct disorder, autism spectrum disorders, eating disorders, attention-deficit hyperactivity disorder (ADHD), and other mental disorders (8). Among these, schizophrenia is one of the most common and burdensome psychiatric disorders in adults worldwide (9). Some previous DUR indicates that schizophrenia (6, 7, 10) and depression (11, 12) were commonly encountered psychiatric disorders in India.
Irrational prescribing is a global problem. Prescribing errors promote irrational use of drugs, decrease patient compliance, and increase the cost and duration of the treatment. Such practices also lead to the emergence of drug interactions, drug resistance, and adverse drug reactions, which increases the rate of mortality and morbidity (13). Psychotropic medications prescribed to manage psychiatric disorders usually follow the guidelines formulated by various organizations. However, it is often discussed that many patients receive irrational prescriptions, which either do not provide any benefit to the patients or harm them (14). Psychiatric illnesses are chronic and may profoundly impact the sufferer's quality of life, family members, and society (15). The problem may compound with inappropriate and irrational prescribing.
In the form of DUR, periodic prescription audits can improve rational prescribing and prescription quality. Keeping in view the principle aim of DUR to facilitate the rational use of drugs in the population, this study was undertaken to investigate the prescription pattern of psychotropic drugs and also to assess the rationality of the prescriptions in an outpatient department of psychiatry unit in a tertiary care teaching hospital in Assam.
Materials and Methods
Study Design
The study was a hospital-based, non-interventional, prospective, cross-sectional study conducted at the Department of Psychiatry. Further analysis was conducted in the Department of Pharmacology, Assam Medical College and Hospital (AMCH). The study was conducted after approval of the Institutional Ethics Committee (H) (AMC/EC/2777-Dt 25/05/2022), for 6 months, from August 1, 2022, to January 31, 2023.
Selection Criteria
All new OPD patients of any age and gender on a psychiatric prescription and those consented to participate in the study were included. Patients who refused to participate and prescriptions that did not contain any psychotropic drugs were excluded.
Data Collection Method
The data collection method was individual consultations. All participating patients received a patient information card, and informed consent was obtained in their native language. Data were collected through direct observation in a specially designed form containing relevant details such as patient demographics, prescription information, diagnosis, and prescription details- hospital prescription number, date, medication number, generic names/individual brand names and any fixed-dose combinations (FDCs) prescribed.
Sample Size
The sample size was determined using Eq. 1 (16). Where n is the sample size, z is the standard deviation and is fixed at 1.96 for a 95% Confidence interval, Ɛ is the desired level of precision (i.e., the margin of sampling error tolerated), and is fixed at 5% (0.05), p is prevalence.
Equation 1
No previous studies related to DUR were conducted in the Department of Psychiatry, AMCH. To calculate the prevalence of new patients prescribed psychotropic drugs, previous OPD prescriptions (June 2020 – May 2021) of the Psychiatry department were collected from Medical Record Department, analyzed, and found to be around 41%. Taking this as prevalence and with a desired precision of around 5% and 95% Confidence Interval, the calculated sample size was about 371. However, 655 samples were collected as per WHO guidelines, which mention that at least 600 encounters to be included in a cross-sectional survey, with a greater number if possible (17).
Data Analysis
For measuring WHO core prescribing indicators, WHO /INRUD (International Network of Rational Use of Drugs) guidelines were followed (17). To assess the rational use of drugs, the mathematical model developed and validated by Zhang and Zhi (18) was applied to appraise medical care comprehensively. This method was used in various medical and health research, called the Index of Rational Drug Prescribing (IRDP) (19). There are five indicators of rational drug prescribing from which the optimal prescribing indicators were defined. Prescriptions with five or more drugs were defined as polypharmacy. These five prescribing indicators (prescriptions including antibiotics, polypharmacy prescription, prescriptions including injection, drugs prescribed by generic name, and drugs prescribed from National List of Essential Medicines of India (NLEM)(19) had the same optimal index of 1. A prescription is considered more rational; when it’s all prescribing indicators are closer to 1. The Index of Rational Drug Prescribing (IRDP) was calculated by adding the index values of all prescribing indicators. Based on the index values, IRDP was defined (19, 20). For the calculated indices; index of non-polypharmacy (NP), index of rational antibiotic use (RA), and index of safe injection use (SI), Eq. 2 was used. On the other hand, Eq. 3 was used to calculate the other indices, index of generic name(GN) and index of prescription from NLEM (20).
Equation 2
Equation 3
Statistical Analysis
Standard prescriptions, patient care, and facility-specific indicators were used for data analysis. Data reliability was ensured by following WHO guidelines and methods (17). The results are presented with descriptive statistics such as percentages, ratios, or averages. The data was recorded and evaluated with Microsoft Excel 2007.
Results
Characteristics of Study Participants
A total of 655 prescriptions were analyzed, comprising a demographic split where 54.96% were Male participants and 45.04% were Female participants. Interestingly, the prevalence of psychiatric illnesses, amounting to 27.79%, was notably concentrated within the age group of 21 to 50 years across both sexes. The relative distribution of various psychiatric disorders across different age groups and genders is detailed in Table 1, providing a comprehensive view of these trends within the analyzed dataset.
The Pattern of Psychiatric Disorders
The percentage of prescriptions for schizophrenia, bipolar mood disorders, major depression, anxiety disorders and alcohol-related disorders were 37.86%, 4.88%,11.30%,10.23% and 18.78% respectively. Psychiatric illnesses like erectile dysfunction, premature ejaculation, panic disorders, neuropathy, sleep disturbances, seizure disorders, ADHD, internet addiction, stress-related disorders, dementia/alzheimer's disease, other substance abuse, mental retardation, post-stroke sequelae, and personality disorders – were grouped as ‘other psychiatric illnesses (16.95%). The morbidity pattern and sex difference among different psychiatric illnesses are summarized in Table 2.
Table 1. Age and gender-wise distribution of psychiatric disorders.
|
Psychiatric Disorder |
Age group in Years |
Gender |
|||||||
|
0-10 |
11-20 |
21-30 |
31-40 |
41-50 |
51-60 |
˃60 |
Male |
Female |
|
|
Schizophrenia and other Psychoses (n=248) |
0 |
29 |
74 |
62 |
46 |
18 |
19 |
121 |
127 |
|
Bipolar Mood Disorders (n=32) |
0 |
6 |
12 |
8 |
1 |
5 |
0 |
23 |
9 |
|
Anxiety Disorder (n=67) |
0 |
10 |
22 |
17 |
12 |
3 |
3 |
30 |
37 |
|
Major Depression (n=74) |
0 |
7 |
23 |
14 |
18 |
8 |
4 |
36 |
38 |
|
Alcohol-related Disorder ( n=123) |
0 |
1 |
20 |
52 |
38 |
9 |
3 |
117 |
6 |
|
Others (n=111) |
6 |
23 |
31 |
16 |
17 |
10 |
8 |
33 |
78 |
|
Total (n= 655) |
6 |
76 |
182 |
169 |
132 |
53 |
37 |
360 |
295 |
Table 2. Morbidity pattern and sex difference among different psychiatric illnesses.
|
Diagnosis |
Male [n(%)] |
Female [n(%)] |
Total [n(%)] |
|
Schizophrenia and other Psychoses |
121(18.47) |
127(19.39) |
248 (37.86) |
|
Bipolar Mood Disorders |
23(3.51) |
9(1.37) |
32(4.88) |
|
Anxiety Disorder |
30(4.58) |
37(5.65) |
67 (10.23) |
|
Major Depression |
36(5.50) |
38(5.80) |
74 (11.30) |
|
Alcohol-related Disorder |
117(17.86) |
6(0.92) |
123(18.78) |
|
Other psychiatric illnesses |
33(5.04) |
78(11.91) |
111(16.95) |
|
Total |
360(54.96) |
295(45.04) |
655 (100) |
Table 3. WHO core drug prescribing indicators.
|
No. |
Prescribing indicators |
Optimal values |
Results |
|
1. |
Average number of drugs per encounter (n) |
1.6-1.8 |
2.58 |
|
2. |
Percentage of drugs prescribed by generic name (%) |
100 |
39.80 |
|
3. |
Percentage of encounters with an antibiotic prescribed (%) |
20.0-26.8 |
0.00 |
|
4. |
Percentage of encounters with an injection prescribed (%) |
13.4-24.1 |
1.00 |
|
5. |
Percentage of drugs prescribed from NLEM (%) |
100 |
48.49 |
|
Patient Care Indicators |
|||
|
1. |
Average consultation time (min) |
≥10 |
13.78 |
|
2. |
Average dispensing time (sec) |
≥90 |
377 |
|
3. |
Percentage of drugs dispensed (%) |
100 |
61.53 |
|
4. |
Percentage of drugs adequately labeled (%) |
100 |
100 |
|
5. |
Percentage of patients' knowledge of correct dosage (%) |
100 |
44.03 |
|
Health Facility Indicators |
|||
|
1. |
Availability of a Copy of the National List of Essential Medicines of India (NLEM) |
100 |
Yes |
|
2. |
Availability of key drugs (%) |
100 |
66.08 |
Table 4. Use of psychotropic drugs in different psychiatric illnesses.
|
Drugs Groups |
Schizophrenia and other Psychoses % (n=248) |
Bipolar Mood Disorders % (n=32) |
Anxiety Disorder % (n=67) |
Major Depression % (n=74) |
Alcohol-related Disorder % (n=123) |
Others % (n=111) |
Total (n= 655) [n(%)] |
|
Antianxiety drugs |
122 |
14 |
50 |
38 |
102 |
70 |
396(60.4) |
|
Antipsychotic drugs Atypical Typical Total |
262 30
|
37 1 |
6 3 |
12 3
|
19 4 |
40 0 |
379(57.86) 78(11.91) 457(69.77) |
|
Antidepressant drugs SSRI TCA Atypical Others Total |
18 1 2 1 |
2 0 1 0 |
47 0 0 2 |
52 7 17 4 |
4 0 1 0 |
20 1 1 2 |
143(21.83) 9(1.84) 22(3.36) 9(1.84) 183(27.93) |
|
Mood stabilizers Lithium Alternative drugs Total |
0 7 |
1 12 |
0 0 0 |
0 0 0 |
0 0 0 |
0 0 0 |
1(0.15) 19(2.9) 20(3.05) |
|
Anticholinergic drugs |
86 |
0 |
0 |
6 |
4 |
9 |
112(17.09) |
|
Anti ChE |
2 |
0 |
0 |
0 |
0 |
3 |
7(1.07) |
Analysis of Prescription Patterns According to Various WHO/INRUD Drug Use Indicators
The 655 prescriptions contained a total of 1691 drugs. Out of these, 1074 were psychotropic drugs. The other drugs commonly co-prescribed were Vitamin D3, Vitamin B12, Ursodeoxycholic Acid, Melatonin, Benfotiamine, Pantoprazole, Calcium, Silymarine, and Multivitamins/Multimineral. There was no prescription for more than five drugs.
Table 3 summarizes the Prescription Patterns According to Various WHO / INRUD Drug Use Indicators. Table 4 summarizes the use of psychotropic drugs in different psychiatric illnesses. The most frequently encountered psychotropic medications were the antianxiety drugs in all groups of psychiatric illnesses.
The total numbers of drugs that were prescribed in OPD were 45 nos. Out of these, 35 nos. of drugs were from the psychotropic group: Antianxiety drugs (lorazepam, alprazolam, etizolam, zolpidem, oxazepam, chlordiazepoxide, propranolol, clobazam, clonazepam); Antipsychotic drugs (Atypical: olanzapine, risperidone, clozapine, aripiprazole, quetiapine; Typical: amisulpride, flupenthixol, fluphenazine); Antidepressant drugs (SSRI: escitalopram, citalopram, sertraline, fluoxetine, fluvoxamine, paroxetine; TCA: amitriptyline; Atypical: mirtazapine; Others: desvenlafaxine, vortioxetine); Mood Stabilizers: ( lithium, Alternative drugs: sodium valproate, carbamazepine, oxcarbazepine); Anticholinergic drugs: trihexyphenidyl, benzhexol); Anti ChE:( donepezil); Anti-craving drug (baclofen, acomprosate).
Fixed Dose Combinations of Psychotropic Drugs (FDCs)
In the examined population, a variety of fixed-dose combinations (FDCs) comprising psychotropic drugs were identified in the prescribed regimens. These included risperidone 3 mg plus trihexyphenidyl 2 mg, which was administered to 62 patients. Similarly, risperidone 2 mg plus trihexyphenidyl 2 mg was prescribed to 19 patients, while risperidone 4 mg plus trihexyphenidyl 3 mg was prescribed to 9 patients. Furthermore, paroxetine 12.5 mg plus clonazepam 0.25 mg was observed in the treatment of 2 patients, alongside paroxetine 12.5 mg plus clonazepam 0.5 mg also prescribed to 2 patients. Another combination, escitalopram 10 mg plus clonazepam 0.5 mg, was utilized in the management of 16 patients, whereas escitalopram 10 mg plus clonazepam 0.25 mg was employed in the treatment of 2 patients. Additional FDCs included fluoxetine 20 mg plus olanzapine 5 mg, which was prescribed to 4 patients, and propranolol 20 mg plus clonazepam 0.5 mg, administered to 3 patients. These findings demonstrate the diverse range of FDCs utilized in the pharmacological management of psychiatric conditions within the studied population.
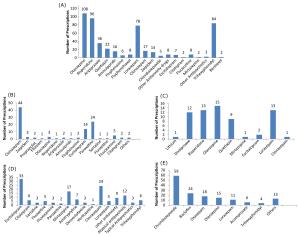
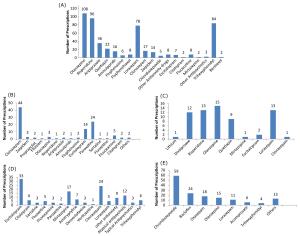
Drugs Used in Various Psychiatric Disorders
Figure 1 provides an overview of the pharmacological treatment options used in a range of psychiatric disorders. It highlights the drugs prescribed specifically for schizophrenia and other psychosis (Figure 1A), anxiety disorder (Figure 1B), bipolar disorder (Figure 1C), major depression (Figure 1D), and alcohol-related disorder (Figure 1E). This comprehensive visual representation serves to illustrate the diverse array of medications employed in the management of these psychiatric conditions.
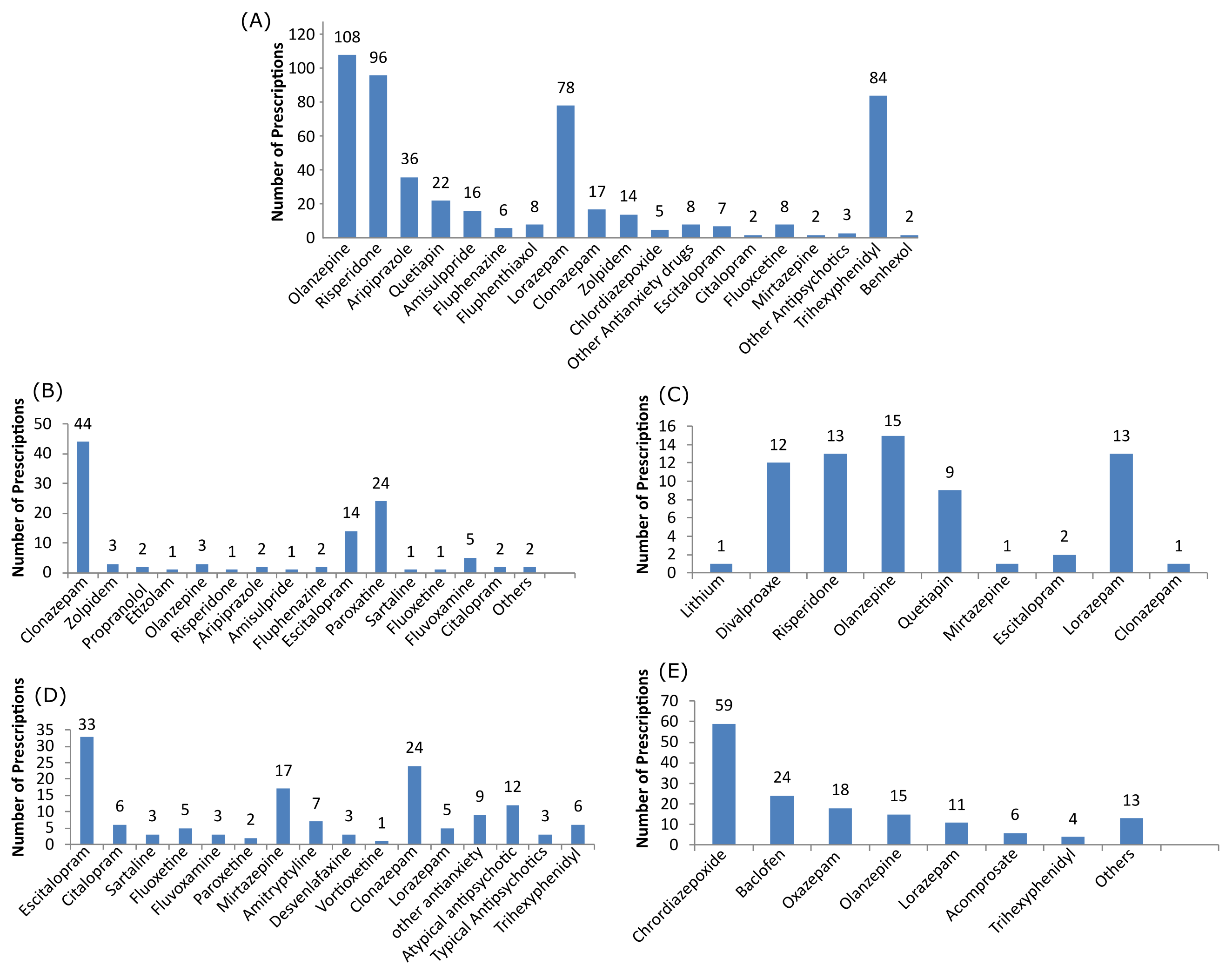
Figure 1. Drugs prescribed in schizophrenia and other psychosis (A), anxiety disorder (B), bipolar disorder (C), major depression (D) and alcohol-related disorder (E). Note: X-axis is the prescribed drug's name.
Table 5. Optimal levels of prescribing drug indicators and IRDP value.
|
Prescribing indicators |
Optimal level (%) |
Optimal index |
Observed value (%) |
Index of rational drug prescribing |
Indices |
|
Prescriptions including antibiotic |
<30 |
1 |
0 |
Rational antibiotic index |
1 |
|
Polypharmacy prescription |
0 |
1 |
0 |
Index of polypharmacy |
1 |
|
Prescriptions including injection |
<10 |
1 |
1 |
Index of safety injection |
1 |
|
Drugs prescribed by generic name |
100 |
1 |
39.80 |
Generic name index |
0.39 |
|
Drugs prescribed by NLEM |
100 |
1 |
48.49 |
NLEM index |
0.48 |
|
Total calculated IRDP value |
|
5 |
|
|
3.87 |
Index of Rational Drug Prescribing (IRDP) The overall IRDP of the present study was 3.87, with an optimal level of 5 (Table 5). The overall IRDP of 3.87 was made up of adding the index of antibiotic 1, index of polypharmacy 1, index of injection 1, index of generic name 0.39, and drugs from NLEM 0.48 (19-21).
Discussion
Study Participants
Male patients (54.96%) frequently visited psychiatric OPD compared to female patients (45.04%). Many studies have shown similar results of male preponderance (4, 6, 7). The reproductive age group (20–40 years) accounted for the majority (73.74%) of all psychiatric disorders, as has been seen in many other studies (4, 6). In this study, schizophrenia and other psychoses were the most common diagnosis, followed by alcohol-related disorders, depression, anxiety disorders and bipolar mood disorder (Table 2). Piparva et al. (7) have found that schizophrenia was the most common diagnosis, followed by depression whereas, in this study, alcohol-related disorder came in second with a male preponderance, with the age group of 21-50 years.
Analysis of Prescriptions as per the WHO/INRUD Drug
Used Indicators
The average number of prescription drugs was 2.58, which was similar to other studies (4, 6, 7). A maximum of five drugs were prescribed in a few prescriptions where other co-morbidities were present. Otherwise, no polypharmacy was observed. Polypharmacy can lead to poor compliance, drug interactions, and adverse drug reactions. It is a growing global issue affecting primary and secondary care, predominantly driven by an aging, multimorbid population coupled with the increasing use of evidence-based clinical guidelines (22). WHO’s “Medication without Harm –Global patient safety challenge” targets one of the most pressing public health issues of present times: iatrogenic harm. Multimorbidity, polypharmacy, and fragmented health care (i.e., patients attending appointments with multiple physicians in various healthcare settings) are key drivers of medication-related harm, which can result in negative functional outcomes, high hospitalization rates, and excess morbidity and mortality (23). Generic names were prescribed for 39.80% of total drugs. The reason behind more branded medication in this study may be clinicians' belief that the therapeutic equivalence of generic drugs is unproven, and patients may believe they are getting inferior drugs (24). However, if adequate quality control is assured, generic substitution can benefit the patient. In this study, injections (1.00%) prescribed were lorazepam, fluphenazine, haloperidol decanoate 5 mg, promethazine, thiamine, olanzapine, pantoprazole, ondansetron in people with schizophrenia, and other alcohol-related disorders. Several Indian studies have evaluated the efficacy of depot antipsychotics in schizophrenia and found their usefulness in treating acute schizophrenia and as maintenance therapy. Concerns about the side effects and economics of the drug's parenteral administration probably explain the depot injection's low use (25). 48.49% of the drugs were prescribed by the National Essential Medicines List of India 2022. The main goal of the NLEM is to promote the rational use of medicines, considering three important aspects: cost, safety, and effectiveness. In addition, it will also encourage the prescription of drugs with their generic names (26).
Observed Prescription Pattern in Schizophrenia
In our study, the most commonly prescribed drugs were atypical antipsychotics (89.73%), olanzapine (36.98%), followed by risperidone (32.87%) in comparison with typical antipsychotics (10.27%). No single prescription was observed for clozapine and ziprasidone in the study group (Figure 1). In diagnosed schizophrenia and other psychoses, lorazepam (63.93%) was prescribed, followed by clonazepam (13.93%). Guidelines for the rational use of benzodiazepines recommend short-term use (maximum 4 weeks) or intermittent treatments with minimally effective doses, which should be prescribed only for severe symptoms. (27). Some studies found that first-generation drugs are just as useful as second-generation drugs, except for clozapine, which is superior to all of them (28). Jones PB et al. concluded that initiating treatment with typical rather than atypical antipsychotics in people with schizophrenia whose medication was changed due to intolerance or inadequate response over one year had no adverse effects on quality of life, symptoms, or related outcomes associated with care costs (29). In patients with chronic schizophrenia, olanzapine was more effective than the other drugs tested, and no significant differences in effectiveness were found between the conventional drug perphenazine and the other second-generation drugs. Olanzapine has been associated with increased weight gain, HbA1C, cholesterol, and triglycerides and has been responsible for metabolic syndrome(30). The 2010 National Institute of Clinical Excellence (NICE) guidelines suggested that it is not necessary to prescribe an "atypical" drug as a first-line treatment, and clozapine can only be offered after the primary failure of two antipsychotics (31).
Observed Prescription Patterns in Bipolar Mood Disorders
For bipolar mood disorder, Divalproex was prescribed most frequently (23.53%). Lithium was found in only one prescription. Second-generation antipsychotics prescribed were olanzapine (29.41%), followed by risperidone (25.4%).49%), and quetiapine (17.65%). Studies have shown that extreme states of mania and depression can be managed with mood-stabilizing medications, which can reduce the number of manic and depressive episodes. Kessing et al. found that lithium is superior to valproate in general (32), having the most robust evidence of long-term relapse prevention, and is the first-line treatment for both acute and maintenance treatment of bipolar mood disorder. Despite its global therapeutic use, the benefits of lithium are restricted by its narrow therapeutic index and the incidence of adverse effects (33). Concerns about the narrow therapeutic index and difficulties in monitoring serum lithium concentrations at our facility explain the low lithium consumption observed in this study.
Observed Prescription Pattern in Major Depression
Among the antidepressants, escitalopram (41.25%) was the most commonly prescribed drug, followed by mirtazapine (21.25%) and amitriptyline (8.75%). Overall, SSRIs (65%) were prescribed more often than TCAs (8.75%). This is consistent with current recommendations (APA guidelines) and practices for treating mood disorders, which recommend a second-generation antidepressant due to the reduced risk of side effects (34). According to guidelines from the American College of Physicians, all of these agents have similar efficacy, and the choice of different second-generation antidepressants should be based on side effects, cost, and patient preference. Patient response to treatment and side effects of antidepressants should be assessed within 1-2 weeks of starting treatment (35).
Observed Prescription Patterns in Anxiety
Disorders
Clonazepam (44.44%) was the most commonly prescribed antianxiety drug, followed by SSRI - paroxetine (24.24%), escitalopram (14.14%), and others (17.18%). The NICE guidelines for treating anxiety disorders state that SSRIs, or serotonin-norepinephrine reuptake inhibitors (SNRIs), should be a first choice.
In general, benzodiazepines should be avoided and used only briefly in times of crisis (36). Combining a benzodiazepine with an SSRI may provide faster anxiety control, reduction in SSRI-induced anxiety or agitation that may occur early in treatment, better antidepressant adherence, and better control of episodic or situational anxiety in response to specific stimuli. These benefits must be weighed against the potential risks of combination therapy, including side effects, drug abuse, and potential worsening of depressive symptoms(37). Alprazolam and lorazepam were not used for anxiety disorders, as evident from the prescriptions in this study.
Observed Prescription Patterns in Alcohol-related
Disorders (ARDs)
In this study, the incidence of ARDs was high (18.78%). Chlordiazepoxide (39.33%) was the most commonly prescribed antianxiety drug for ARD, followed by oxazepam (12%), lorazepam (7.33%), and atypical antipsychotic olanzapine (10%). Other drugs commonly prescribed for ARDs were ursodeoxycholic acid, baclofen, acamprosate, and pantoprazole. Alcohol use has increased globally, with varying trends in different parts of the world, and has been identified as one of the ten leading risk factors for the burden of disease. There have been a series of global initiatives to reduce the harmful use of alcohol, including WHO’s global strategy to reduce the harmful use of alcohol (38).
Central anticholinergic drug trihexyphenidyl (a few Benhexol) was prescribed in various psychiatric illnesses and was found to be the maximum in schizophrenia (75.44%). They are recommended to avoid extrapyramidal side effects (EPS) associated with typical antipsychotics. In schizophrenia, the prescribing frequency of atypical antipsychotics (57.86%) was higher than the typical one (11.91%), and most patients were prescribed anticholinergic agents. Co-prescribing of anticholinergic drugs may add to new or additive adverse effects (e.g., dry mouth, blurred vision, constipation), further reducing the quality of life. As routine use of anticholinergic agents adds to the complexity, side effects, and expenses, whether they should be prescribed routinely or reserved for the cases of overt EPS remains open to question (7). WHO does not recommend anticholinergics to be used routinely for preventing EPS in psychotic disorders treated with antipsychotics. Short-term use of anticholinergics may be considered only in individuals with significant EPS when dose reduction and switching strategies have proven ineffective or when these side effects are acute or severe (39).
FDCs have advantages and disadvantages, susceptibility for EPS differs from person to person, and not all patients require the addition of trihexyphenidyl to overcome EPS. Moreover, the antipsychotic-anticholinergic combination does not permit the need-based dose titration of trihexyphenidyl. This could cause additional peripheral and central anticholinergic side effects in the patients, and the long-term use of trihexyphenidyl may cause cognitive impairment and tardive dyskinesia (39).
An interesting case has come to light in which a 14-year-old boy with internet addiction disorder (IAD) was counseled with behavioral therapy. Cognitive behavioral therapy shows promising results in IAD. Methylphenidate reduces internet usage time in children with IAD co-existing with ADHD (40). However, there is still no consensus on which treatment to offer first.
Conclusion
In this study, the use of psychotropic drugs for different indications followed current guidelines despite the low prevalence of generic prescribing. There is no gender and age difference in prescribing pattern. No polypharmacy was seen, and the use of FDCs was also less. Antianxiety drug lorazepam was extensively prescribed in almost all types of psychiatric illnesses, with a maximum percentage in anxiety and schizophrenia. Rational use of Benzodiazepines requires attention in terms of dose and duration. Atypical antipsychotic olanzapine was more frequently prescribed. Prescribing frequency and pattern of the central anticholinergic drug were similar to antipsychotic drugs irrespective of typical or atypical. Routine use of trihexyphenidyl along with atypical antipsychotic drugs is not justified. The increasing number of alcohol-related disorders in young adults is also a great concern. DUR is an effective tool to promote rational drug prescribing. Despite all the limitations, such as small sample size, shorter study duration, single study center, etc., the study may be an eye-opener for the healthcare provider. Conducting similar studies on larger study populations will further strengthen the database regarding the drug utilization research of psychotropic drugs.
Declarations
Acknowledgment
The authors would like to thank the Professor and Head of the Department of Psychiatry, all the resident physicians, postgraduate trainees, and OPD staff of the Psychiatry Department Assam Medical College and Hospital, Dibrugarh, Assam, for their constant support and guidance.
Ethics Statement
The study was approved by the Institutional Ethics Committee of Assam Medical College with approval letter number of AMC/EC/2777-Dt 25/05/2022.
Data Availability
You can access the Supplemental Table on the ETFLIN server via the following link: https://etflin.com/file/document/20230607063455822779719.xlsx
Funding Information
Not applicable.
Conflict of Interest
The authors declare no conflicting interest.
References
- WHO. Introduction to Drug Utilization Research. WHO International Working Group for Drug Statistics Methodology, WHO Collaborating Centre for Drug Statistics Methodology, WHO Collaborating Centre for Drug Utilization Research and Clinical Pharmacological Services. World Health Organization Oslo, Norway. 2003. https://apps.who.int/iris/handle/10665/42627
- Sachdeva PD, Patel BG. Drug Utilization Studies-Scope and Future Perspectives. Int J Pharm Biol Res. 2010;1(1):11–7.
- GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet Psychiatry. 2022;9(2):137–50.
- Chawla S, Agarwal M, Sharma S, Jiloha RC. Drug utilization study of psychotropic drugs among psychiatric outpatients in a tertiary care hospital. Indian J Pharm Sci. 2017;79(6):1008–13.
- Pincus HA, Tanielian TL, Marcus SC, Olfson M, Zarin DA, Thompson J, et al. Prescribing trends in psychotropic medications: Primary care, psychiatry, and other medical specialties. JAMA. 1998;279(7):526–31.
- Mudhaliar MR, Ghouse ISM, Sadubugga P, Narala SR, Chinnakotla V, Yendluri P. Psychotropic drug utilization in psychiatric outpatient department of a tertiary care teaching hospital in India. Int J Res Med Sci. 2017 Mar 28;5(4):1612–6.
- Piparva KG, Parmar DM, Singh AP, Gajera M V., Trivedi HR. Drug utilization study of psychotropic drugs in outdoor patients in a teaching hospital. Indian J Psychol Med. 2011; 33(1):54–8.
- Sagar R, Dandona R, Gururaj G, Dhaliwal RS, Singh A, Ferrari A, et al. The burden of mental disorders across the states of India: the Global Burden of Disease Study 1990–2017. The Lancet Psychiatry. 2020;7(2):148–61.
- Huhn M, Nikolakopoulou A, Schneider-Thoma J, Krause M, Samara M, Peter N, et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Lancet. 2019;394(10202):939–51.
- Bodke P, Bhosle R. Psychotropic drugs utilization pattern at tertiary care institute - a retrospective analysis. Int J Recent trends Sci Technol. 2014;11(3):400–3.
- Ilyaz M, Baig MMA, Ramakrishna, Quadir MA, Fathima M, Khan SAS. Drug utilization study of antipsychotics and its common ADR’S in the psychiatry OPD of OHRC. Int J Pharm Pharm Sci. 2014;6(9):162–5.
- Mukherjee S, Sen S, Chatterjee SS, Biswas A, Sinha S, Ghosal M, et al. Prescribing Pattern of Psychotropic Medications in Psychiatry Outpatients at a Tertiary Care Teaching Hospital in India: A Prospective Cross-sectional Study. Int J Hosp Res. 2014;3(3):113–22.
- Singh T, Banerjee B, Garg S, Sharma S. A prescription audit using the World Health Organization‑recommended core drug use indicators in a rural hospital of Delhi. J Educ Health Promot. 2019;8(February):1–5.
- Grover S, Avasthi A, Sinha V, Lakdawala B, Bathla M, Sethi S, et al. Indian Psychiatric Society multicentric study: Prescription patterns of psychotropics in India. Indian J Psychiatry. 2014;56(3):253–64.
- Iseselo MK, Kajula L, Yahya-Malima KI. The psychosocial problems of families caring for relatives with mental illnesses and their coping strategies: A qualitative urban based study in Dar es Salaam, Tanzania. BMC Psychiatry. 2016;16(1):1–12.
- Demeke B, Molla F, Assen A, Melkam W, Abrha S, Masresha B, et al. Evaluation of drugs utilization pattern using who prescribing indicators in Ayder Referral Hospital, Northern Ethiopia. Int J Pharma Sci Res. 2015;6(2):343–7.
- WHO. How to investigate drug use in health facilities. Selected drug use indicators. https://apps.who.int/iris/handle/10665/60519.
- Zhang Y, Zhi M. Index system, appraising method for comprehensive appraisal. J North Jiaotong Univ. 1995;19.
- Dong L, Yan H, Wang D. Drug prescribing indicators in village health clinics across 10 provinces of Western China. Fam Pract. 2011;28(1):63–7.
- Atif M, Sarwar MR, Azeem M, Naz M, Amir S, Nazir K. Assessment of core drug use indicators using WHO/INRUD methodology at primary healthcare centers in Bahawalpur, Pakistan. BMC Health Serv Res. 2016;16(1).
- El Mahalli AA, Akl OAM, Al-Dawood SF, Al-Nehab AA, Al-Kubaish HA, Al-Saeed SI, et al. 1086 WHO/INRUD patient care and facility-specific drug use indicators at primary health care centres in Eastern province, Saudi Arabia. East Mediterr Heal J. 2012;18(11):1086–90.
- Payne RA. The epidemiology of polypharmacy. Clinical Medicine. 2016;16(5):465.
- Daunt R, Curtin D, O'Mahony D. Polypharmacy stewardship: a novel approach to tackle a major public health crisis. The Lancet Healthy Longevity. 2023 May 1;4(5):e228-35.
- Duerden MG, Hughes DA. Generic and therapeutic substitutions in the UK: Are they a good thing? Br J Clin Pharmacol. 2010;70(3):335–41.
- Avasthi A, Aggarwal M, Grover S, Khan MKR. Research on antipsychotics in India. Indian J Psychiatry. 2010;52(S3):17–40.
- NLEM 2011. https://pharmaceuticals.gov.in/sites/default/files/NLEM.pdf.
- Ashton H. Guidelines for the rational use of benzodiazepines: when and what to use. Drugs. 1994;48(1):25–40. doi: 10.2165/00003495-199448010-00004. PMID: 7525193.
- Lieberman JA, Stroup TS. The NIMH-CATIE Schizophrenia Study: what did we learn?. American Journal of Psychiatry. 2011 Aug;168(8):770-5.
- Jones PB, Barnes TRE, Davies L, Dunn G, Lloyd H, Hayhurst KP, et al. Randomized controlled trial of the effect on quality of life of second- vs first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS 1). Arch Gen Psychiatry. 2006;63(10):1079–87.
- Lieberman JA, Stroup TS, Mcevoy JP, Swartz MS, Rosenheck RA, Perkins DO, et al. Effectiveness of Antipsychotic Drugs in Patients with Chronic Schizophrenia. New England journal of medicine. 2005 Sep 22;353(12):1209-23.
- National Collaborating Centre for Mental Health (UK). Psychosis and Schizophrenia in Adults: Treatment and Management: Updated Edition 2014. London: National Institute for Health and Care Excellence (UK); 2014. (NICE Clinical Guidelines, No. 178.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK248060/
- Kessing LV, Hellmund G, Geddes JR, Goodwin GM, Andersen PK. Valproate v. lithium in the treatment of bipolar disorder in clinical practice: observational nationwide register-based cohort study. Br J Psychiatry. 2011;199(1):57–63.
- Sheikh M, Qassem M, Triantis IF, Kyriacou PA. Advances in Therapeutic Monitoring of Lithium in the Management of Bipolar Disorder. Sensors. 2022;22(3):736-63.
- American Psychological Association. (2019). Clinical practice guideline for the treatment of depression across three age cohorts. https://www.apa.org/depression-guideline
- Qaseem A, Snow V, Denberg TD, Forciea MA, Owens DK. Using second-generation antidepressants to treat depressive disorders: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2008;149(10):725–33. https://pubmed.ncbi.nlm.nih.gov/19017591/
- Common mental health disorders - Identification and pathways to care: NICE clinical guideline 2021. National Clinical Guideline Number 123. National Collaborating Centre for Mental Health Commissioned by the National Institute for Health and Clinical Excellence. www.nice.org.uk/guidance/cg123/chapter/1-Guidance
- Dunlop BW, Davis PG. Combination Treatment With Benzodiazepines and SSRIs for Comorbid Anxiety and Depression: A Review. Prim Care Companion J Clin Psychiatry. 2008;10(3):222–8.
- Shield K, Manthey J, Rylett M, Probst C, Wettlaufer A, Parry CDH, et al. National, regional, and global burdens of disease from 2000 to 2016 attributable to alcohol use: a comparative risk assessment study. Lancet Public Heal. 2020;5(1):e51–61.
- WHO. Individuals with psychotic disorders ( including schizophrenia ) who require long term antipsychotic treatment , are anticholinergic medications more effective in preventing or reducing extrapyramidal side ‐ effects and / or improving treatment. https://cdn.who.int/media/docs/default-source/mental-health/mhgap/psychosis-and-bipolar-disorders/role-of-anticholinergic-medications-in-patients-requiring-long-term-antipsychotic-treatment-for-psychotic-disorders.pdf?sfvrsn=68417542_0
- Cash H, Rae CD, Steel AH, Winkler A. Internet Addiction A Brief Summary of Research and Practice. Curr Psychiatry Rev. 2012;8(4):292–8.
 ETFLIN
Notification
ETFLIN
Notification