Potential Drug Interactions in Inpatients with Chronic Kidney Disease at Undata Hospital, Palu City, Indonesia
by Indah Kurnia Utami ★ , Niluh Puspita Dewi, Syafika Alaydrus, Magfirah Magfirah, Musfirah Musfirah, Nur Azizah
Academic editor: Mohd Shahezwan Abd Wahab
Sciences of Pharmacy 2(4): 243-248 (2023); https://doi.org/10.58920/sciphar02040037
This article is licensed under the Creative Commons Attribution (CC BY) 4.0 International License.
19 Oct 2023
25 Nov 2023
25 Nov 2023
26 Nov 2023
Abstract: Patients with Chronic Kidney Disease (CKD) often receive a combination of medications, which can have beneficial effects but may also lead to ineffective treatment. The objective of this study was to analyze potential drug interactions in CKD patients admitted to the Seroja ward at Undata Hospital in Palu, Central Sulawesi Province, during the year 2022. The study was conducted prospectively from July 20 to September 18, 2022, involving a total of 40 patients. The research utilized a non-experimental observational design, and the results were presented descriptively using purposive sampling based on predefined criteria. Drug interaction were screened using the Drug Interaction Checker tool. The study revealed that among CKD patients, a higher percentage of men (55%) than women (44%) were observed, with the highest percentage in the age group of 46–55 (27.5%). The most commonly drug group used was loop diuretics and furosemide (18.75%). The most significant potential drug interactions were pharmacodynamic interactions (12.5% in 5 cases) with minor significance, followed by pharmacokinetic interactions (2.5% in 1 case) with major significance, particularly in the use of calcium channel blockers (CCBs) and statins. Based on the findings, minor interaction cases do not always yield negative outcomes. In certain clinical practices, these interactions are intentionally utilized to achieve favorable results. Instances of major interactions with drug use should be avoided, and alternative drugs should be considered. In urgent situations where the drug is necessary, restrictions can be applied, and close monitoring of the patient's clinical status is vital.
Keywords: Drug related problemDrug interactionChronic kidney diseasePharmacodynamic drug interactionPharmacokinetics drug interaction
Introduction
Kidney plays a vital role in the body's metabolic system, participating in numerous activities that can affect its performance when not adequately cared for. Unhealthy lifestyles characterized by the consumption of high-calorie instant foods, inadequate fiber and mineral water intake, and irregular eating patterns exert additional stress on the kidneys. This strain begins with filtration and reabsorption, extending to the augmentation of nutrients transported to the kidneys through the bloodstream (1). Kidney diseases are classified into temporary (Acute Kidney Disease - AKD) and persistent (Chronic Kidney Disease - CKD) types. AKD is characterized by a sudden decline in kidney function, disrupting the body's homeostasis and resulting in increased metabolism of nitrogenous compounds such as urea and creatinine, alongside imbalances in fluid and electrolyte levels (2). On the other hand, CKD signifies a prolonged condition where the body struggles to maintain metabolism and fluid-electrolyte balance, leading to enduring structural and functional damage to the kidneys lasting three months or more (3). The causes of CKD are varied, including conditions such as infection (pyelonephritis), hypertension, metabolic disorders (DM), urinary tract obstruction, immunological disorders, primary tubular disorders (nephrotoxins), and congenital disorders resulting in decreased Glomerular Filtration Rate (GFR) (4).
According to 2018 Riskesdas data, the prevalence of CKD in Central Sulawesi, Indonesia, based on a doctor's diagnosis was 0.52%. The highest incidence was observed in the 55-74 age group (1.67%), male (0.66%), those with elementary school education (0.77%), and individuals residing in rural areas (0.56%) (RISKESDAS, 2018). CKD typically manifests potential complications such as hyperkalemia, heart disease, hypertension, anemia, and bone disease, necessitating a variety of medications tailored to the patient's clinical condition (6). Patients with CKD often require a combination of multiple drugs, with the administration of this drug combination aimed at yielding beneficial effects. However, in certain cases, drug interactions occur, resulting in ineffective treatment and unexpected events. Caution must be exercised in administering drugs to patients with CKD due to the reduced kidney function, impacting drug excretion and metabolism, potentially leading to elevated drug levels in the blood (7).
A substantial number of medication errors stem from inadequate assessment of prescribed drugs, posing a threat to patient morbidity and mortality. Many prescriptions lack thorough evaluation of drug interactions, emphasizing the importance of diligent examination of drug items concerning potential interactions (8). Drug interactions represent one of the eight categories of drug-related problems identified as drug therapy events capable of disrupting optimal clinical outcomes. Hence, pharmacists must possess the expertise to professionally assess and make informed decisions to address these issues (9)
In light of the above insights, it is imperative to identify drug interactions in CKD patients at Undata General Hospital in Central Sulawesi Province using the Medscape feature called ‘Drug Interactions Checker’. This approach enables the determination of potential interactions and their respective levels of occurrence, emphasizing the critical need for a systematic evaluation of drug interactions in this patient population.
Experimental Section
Population and Sample
This research was conducted prospectively in the Seroja room at Undata Hospital, Central Sulawesi Province, from July 20–September 18, 2022. The research design used was an observational, non-experimental study, and the research results were presented descriptively because this study aimed to describe the drug use interactions studied in CKD patients inpatients at the Seroja room at the Undata Hospital in Central Sulawesi Province in 2022. This study has been approved by Ethics Committee of Tadulako University with ethical approval letter number of 4812.A/UN28.1.30/KL/2022.
The sample in this study were patients with a diagnosis of CKD who were given medical therapy according to inclusion-based criteria during the study at the Undata Hospital in Central Sulawesi Province in 2022. The sampling technique used in this study was purposive sampling, namely sampling based on established criteria. All samples that met the requirements are used as appropriate research samples.
In this study, the criteria for inclusion cover individuals aged 18 years or above who have received a diagnosis of Chronic Kidney Disease (CKD). Additionally, included patients must have a minimum length of stay of 3 days in the inpatient room and possess complete and accurate medical record data. Moreover, participation in the research necessitates a willingness to be involved and the act of signing an informed consent form. Furthermore, those who had undergone changes in prescribed drugs and individuals with incomplete medical record data were also excluded from participation.
Data Collection and Analysis
The data collection process in this study employed the purposive sampling technique, a strategic approach to select participants based on specific criteria relevant to the research objectives. Observations were conducted by directly assessing the patients' conditions within the treatment room. Documentation involved utilizing secondary data and extracting relevant information from the patients' medical records. A structured data retrieval sheet was utilized for collecting the necessary data. In instances where data was incomplete, efforts were made to gather comprehensive information. This involved seeking clarification from the patients themselves, their family members, pharmacists, or clinicians involved in their care, ensuring a comprehensive and accurate data collection process. The research findings, derived from this analysis, were then presented in the form of tables and figures, utilizing the collated secondary data. This approach aimed to provide a comprehensive portrayal of the treatment landscape for CKD patients based on the available records.
Result and Discussion
Patients Demography
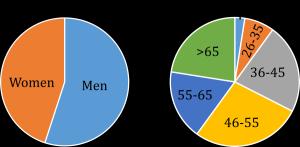
The study's findings, which are derived from data collected in 2022 on Chronic Kidney Disease (CKD) patients hospitalized in the Seroja room of Undata Palu General Hospital, Central Sulawesi Province, revealed a gender-based distribution of CKD patients (see Figure 1). Of the total CKD patients, 22 were men (55%) and 18 were women (45%). These results align with previous research, such as the work by Widhawati and Fitriani (2021), which has suggested that men are more susceptible to CKD (10). This susceptibility is attributed to factors such as occupational hazards, unhealthy lifestyles, and the consumption of supplements that can potentially trigger systemic diseases, leading to a decline in kidney function and a consequent impact on the overall quality of life. Therefore, it is evident that men exhibit a higher susceptibility to CKD when compared to women (11).

Figure 1. Demography of inpatients with chronic kidney disease in Undata Hospital (2022).
Based on the findings presented in Figure 1, the data collected highlights a significant proportion of CKD patients falling within the age group of 46 to 55 years, accounting for 27.5% of the total. This observation is in line with the notion that pre-elderly and elderly age categories represent a higher risk factor for CKD. This association can be attributed to the age-related changes in the body, which may affect creatinine levels. Elevated creatinine levels are often indicative of impaired kidney function, a characteristic feature of kidney disease. Moreover, CKD patients in this age group are more prone to complications that contribute to these higher creatinine levels (12). This phenomenon is further compounded by the natural aging process, which results in the loss of nephrons - the functional units of the kidneys. This loss of nephrons, occurring typically after the age of 40, leads to incomplete filtration of creatinine, consequently causing an increase in creatinine levels. The study's findings underscore the correlation between age, creatinine levels, and the prevalence of CKD, aligning with the insights presented in the research of Widhawati and Fitriani (2021) (10).
Distribution of Prescribed Drugs in Inpatients with Chronic Kidney
Disease
The data from Table 1 revealed the predominant types and classes of drugs used among the study participants. Notably, additional supplements (Aminephron) were administered to 34 patients, constituting 25.56% of the sample, while loop diuretics (Furosemide) were given to 24 patients, representing 18.75% of the total. Additionally, 21 patients (16.40%) received CCB (Amlodipine), and 11 patients (8.59%) were prescribed ARB (Valsartan, Candesartan). It is noteworthy that these drugs are specifically intended for CKD patients.
Table 1. Classification of drugs prescribed in inpatients with chronic kidney disease at Undata Hospital.
|
No. |
Drug Class |
Drug Type |
Drug Amount |
Total |
Percentage (%) |
|
|
Injection |
Tablet |
|||||
|
1. |
Suplemen |
Aminefron (asam amino) |
- |
27 |
34 |
26.56 |
|
Nephrosteril (asam amino) |
7 |
- |
||||
|
2. |
Loop diuretik |
Furosemid |
7 |
17 |
24 |
18.75 |
|
3. |
Angiotensin Reseptor Blocker (ARB) |
Valsartan |
- |
4 |
11 |
8.59 |
|
Candesartan |
- |
7 |
||||
|
4. |
Calcium Channel Blocker (CCB) |
Amlodipin |
- |
21 |
21 |
16.40 |
|
5. |
Beta Blocker |
Bisoprolol |
- |
3 |
5 |
3.90 |
|
V-Block (Carvedilol) |
|
2 |
||||
|
6. |
Insulin |
Novorapid |
4 |
- |
8 |
6.25 |
|
Levemir |
4 |
- |
||||
|
7. |
Nitrat |
ISDN |
- |
3 |
3 |
2.34 |
|
8. |
Anti Anemia |
Lapibal (Mecobalamin) |
8 |
- |
9 |
7.03 |
|
Asam Folat |
- |
1 |
||||
|
9. |
Gout |
Recolfar (Colchicine) |
- |
3 |
7 |
5.46 |
|
Allupurinol |
- |
4 |
||||
|
10. |
Biguanide |
Metformin |
- |
1 |
1 |
0.78 |
|
11. |
Sulfonilurea |
Glimepirid |
- |
1 |
1 |
0.78 |
|
12. |
Statin |
Simvastatin |
- |
2 |
2 |
1.56 |
|
13. |
Anti Platelet |
Clopidogrel |
- |
3 |
3 |
2.34 |
|
14. |
Hemostatik Sistemik |
Vitamin K |
1 |
- |
1 |
0.78 |
|
Total |
31 |
97 |
128 |
100 % |
||
Table 2. Interaction types detected in prescribed drugs in inpatients with chronic kidney disease at Undata Hospital.
|
No |
Interaction Classification |
||
|
Drug Interactions |
Significance Level |
Interaction Mechanism |
|
|
1 |
ARB + Loop Diuretik candesartan + furosemide |
Minor |
Pharmacodynamics |
|
2 |
Beta Blocker + ARB Bisoprolol +candesartan |
Minor |
Pharmacodynamics |
|
3 |
Beta Blocker + CCB Bisoprolol + amlodipin |
Minor |
Pharmacodynamics |
|
4 |
Beta Blocker + Loop diuretic Bisoprolol + Furosemide |
Minor |
Pharmacodynamics |
|
5 |
KSR + Furosemide |
Minor |
Pharmacodynamics |
|
6 |
CCB + Statin Amlodipine + Simvastatine |
Mayor |
Pharmacokinetics |
For instance, Aminephron is prescribed to address kidney function abnormalities in CKD patients. It contains essential amino acids that assist individuals with CKD in meeting their protein intake requirements, while maintaining a low nitrogen content. This dietary approach helps CKD patients by reducing the accumulation of waste materials that their compromised kidneys may struggle to excrete, thus alleviating symptoms of uremia (13).
Furosemide, a loop diuretic, is a preferred therapeutic choice for CKD patients. It can increase sodium expenditure by up to 20% and does not depend on Glomerular Filtration Rate (GFR) for efficacy. Furthermore, it is known for its low incidence of adverse effects. Furosemide is commonly used in CKD patients, particularly those in stages 4-5 undergoing hemodialysis. The primary objective of prescribing furosemide is to inhibit the reabsorption of sodium and chloride, thereby enhancing the excretion of water, sodium, and calcium. This helps in regulating fluid balance within the body and reduces the strain on the heart, facilitating improved blood flow (14).
Potential Drug Interaction
As detailed in Table 2 of the study, the findings indicated the presence of 5 cases characterized as minor drug interactions and 1 case classified as a major drug interaction. These drug interactions hold the potential to affect the effectiveness of the prescribed treatments. However, it is noteworthy that in some clinical scenarios, such interactions are intentionally introduced to achieve favorable outcomes (15).
Among the minor interactions identified, the interaction between candesartan and furosemide is considered beneficial. This is because the presence of loop diuretics, such as furosemide, can help correct hypokalemia, a condition where potassium levels in the blood are too low (16). Additionally, the interaction between Bisoprolol and Candesartan is considered advantageous. Bisoprolol is a selective cardiovascular beta-blocker, primarily affecting β1 adrenergic receptors in the heart. This selectivity ensures that Bisoprolol maximally impacts blood pressure regulation, making it a valuable choice for managing hypertension (17).
On the other hand, the major drug interactions observed involved pharmacokinetic interactions between Simvastatin and Amlodipine. When Amlodipine and Simvastatin are taken together, Amlodipine significantly increases the AUC (area under the curve) of HMG-CoA reductase inhibitors, which includes Simvastatin. This, in turn, elevates simvastatin levels in the body, raising the risk of myopathy or rhabdomyolysis, which are serious muscle-related conditions. Consequently, concurrent use of these drugs is not recommended. If required, the dose of simvastatin should be strictly limited to no more than 20 mg per day, and the patient's clinical status must be closely monitored to ensure their well-being (18).
The study also reveals insights into the classification of drug interactions based on their mechanisms. Notably, 12.5% of the interactions fell into the pharmacokinetic category, while a substantial majority, 87.5%, were classified as pharmacodynamic interactions. This indicates that a significant portion of the potential interactions occurs at the receptor level, within the same physiological context. Such interactions can lead to additive effects (excessive impact), synergistic effects (enhanced influence), or antagonistic effects (opposite actions) (19). This information underscores the complexity of drug interactions and the diverse ways in which they can influence the body's responses to medications.
Furthermore, the potential for pharmacokinetic interactions stands at 2.5% with a major significance level. In situations where major interactions occur, it is advisable to avoid the use of the implicated drugs and instead consider alternative medications. However, if the drug is deemed critically necessary, dose restrictions should be implemented, coupled with close and continuous monitoring of the patient's clinical status to ensure their well-being.
Conclusion
Based on the outcomes of this research, several key conclusions can be drawn regarding the 40 Chronic Kidney Disease (CKD) inpatients in the Seroja room at Undata Hospital, Palu, between July 20 and September 18, 2022. Among these patients, six of them exhibit the potential to experience drug interactions. The most prevalent interactions belong to the pharmacodynamic category, constituting 12.5% with minor significance. It's important to note that minor interaction cases do not necessarily yield negative results. In fact, some clinical practices intentionally introduce such interactions to achieve favorable outcomes. Hence, careful monitoring of drug use is paramount in such cases. These findings highlight the importance of vigilance and careful management in handling drug interactions in CKD patients.
Declarations
Ethics Statement
This study was approved by Ethics Committee of Tadulako University with ethical approval letter number of 4812.A/UN28.1.30/KL/2022.
Data Availability
The unpublished data is available upon request to the corresponding author.
Funding Information
Not applicable.
Conflict of Interest
The authors declare no conflicting interest.
References
- Dicki Alamsyah AP. Sistem Pakar Diagnosa Penyakit Ginjal Menggunakan Metode Forward Chaining Berbasis Android. Int J Artif Intell. 2019;6(1):53–74.
- Maghfiroh AA, Simanjorang C, Simawang AP, Pramesti LT, Wasir R. Faktor-Faktor Yang Berhubungan Dengan Kejadian Gagal Ginjal Akut Pada Anak: a Literature Review. Prepotif J Kesehat Masy. 2023;7(1):41–51.
- Abdullah M. Bethsaida Hospital. 2020. Kenali Penyakit Gagal Ginjal Kronik.
- Guswanti. Asuhan Keperawatan pada Pasien Gagal Ginjal Kronik dengan Hemodialisa di Ruang Flamboyan RSUD Abdul Wahab Sjahrane Samarinda. Prog Retin Eye Res. 2019;561(3):S2–3.
- RISKESDAS. 2018. Departemen Kesehatan Republik Indonesia. Jakarta. 2018;
- Tuloli TS, Mustapa MA, Tuli EP. Evaluasi Penggunaan Obat Pada Pasien Gagal Ginjal Kronik Yang Menjalani Hemodialisis Di Rsud Toto Kabila Periode 2017-2018. Parapemikir J Ilm Farm. 2019;8(2):25–32.
- Makmur SA, Madania M, Rasdianah N. Gambaran Interaksi Obat Pada Pasien Gagal Ginjal Kronik Dalam Proses Hemodialisis. Indones J Pharm Educ. 2022;2(3):218–29.
- Rahayu S. ANALISIS RISIKO INTERAKSI OBAT TERHADAP RESEP PASIEN KLINIK ANAK DI RUMAH SAKIT DI BANJARMASIN ( Risk Analysis Of Drug Interactions On Children Recipes Clinic Patients At Hospitals In Banjarmasin ). J Curr Pharm Sci. 2019;2(2):148–53.
- Rochjana AUH, Jufri M, Andrajati R, Sartika RAD. Masalah Farmasetika dan Interaksi Obat pada Resep Racikan Pasien Pediatri: Studi Retrospektif pada Salah Satu Rumah Sakit di Kabupaten Bogor. Indones J Clin Pharm. 2019;8(1).
- Widhawati R, Fitriani F. Pengaruh Pendidikan Kesehatan Asupan Cairan terhadap Kepatuhan Pembatasan Cairan Pasien Hemodialisis. Faletehan Heal J. 2021;8(02):140–6.
- Harris RC, Zhang MZ. The role of gender disparities in kidney injury. Ann Transl Med. 2020 Apr;8(7):514–514.
- Mallappallil M, Friedman EA, Delano BG, McFarlane SI, Salifu MO. Chronic kidney disease in the elderly: evaluation and management. Clin Pract. 2014 Sep;11(5):525–35.
- Yuniardi AP, Isro’in L, Maghfirah S. Studi Literatur: Edukasi Nutrisi Metode Konseling Intensif Dengan Follow Up Pada Pasien Gagal Ginjal Kronik Dengan Masalah Keperawatan Defisit Nutrisi. Heal Sci J. 2020;4(2):1.
- Hanyaq AT, Ramadhan AM, Samsul E. Kajian Interaksi Obat Pasien Gagal Ginjal Kronis Di Instalasi Rawat Inap Rumah Sakit Samarinda Medika Citra. Proceeding Mulawarman Pharm Conf. 2021;14(14):375–84.
- Niu J, Straubinger RM, Mager DE. Pharmacodynamic Drug–Drug Interactions. Clin Pharmacol Ther. 2019 Jun 26;105(6):1395–406.
- Christina YG. Diajukan untuk Memenuhi Salah Satu Syarat Memperoleh Gelar Sarjana Farmasi (S.Farm. ) Program Studi Farmasi. 2019;
- Husna N, Larasati N. Evaluasi Penggunaan Terapi Antihipertensi Pada Pasien Gagal Ginjal Kronik Dengan Hemodialisis. Media Ilmu Kesehat. 2019;8(1):1–8.
- Wiggins BS, Saseen JJ, Page RL, Reed BN, Sneed K, Kostis JB, et al. Recommendations for Management of Clinically Significant Drug-Drug Interactions With Statins and Select Agents Used in Patients With Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2016 Nov 22;134(21).
- Aprilianti Rakhmadani Gadis, Beta Herilla Sekti LNH. Gambaran Interaksi Obat Penyakit Jantung Koroner dengan Sindroma Metabolik Pada Pasien Rawat Jalan di RS TK II DR. SOEPRAOEN MALANG. J Ris KEFARMASIAN Indones. 2022;4(1):55–73.
 ETFLIN
Notification
ETFLIN
Notification